The decision to intubate – the follow up
3 Jul
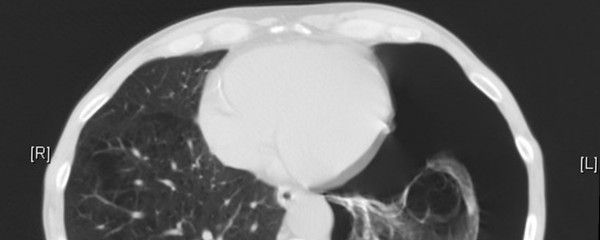
[Image Wikipedia Commons] A few days ago I posted a few cases to try and elicit the reasoning behind why we intubate people. Check out the comments to get a feel for what people were saying. Here’s some follow up. Though … Read More »