Appropriate cardiac cath lab activation: optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction. Am Heart J. 2010 Dec;160(6):995-1003, 1003.e1-8. PMID 21146650 (free full text)
This is a cracking paper that’s worth checking out, especially for the included appendix of ECG examples.
It’s aimed at improving appropriate cath lab activation and talks about some of the more subtle and less widely known STEMI equivalents that are probably surrogates for coronary artery occlusion (the thing we want to activate the cath lab for).
There is of course a much wider issue to do with accurate ECG interpretation and appropriate work-up and diagnosis and possibly even lytic use if you don’t have a cath lab to activate.
Anyhow there’s real pearls in there so let me throw some at you. I’ll assume you’re good with diagnosing a bog-standard inferior or anterior STEMI.
They suggest all of the following may be good candidates be treated as STEMI equivalents:
New (or presumed new) LBBB
- when i first started I was always told that LBBB with chest pain should be treated like a STEMI. This is falling out of favour widely now. 90% of LBBB evaluated in ED do not have MI or need an primary PCI
- the big thing that should get your attention is the Sgarbossa criteria. I’ll not list them here, and they’re of course not perfect but the one thing that always stuck in my mind was concordance – if the ST segment is concordant with the QRS then think STEMI
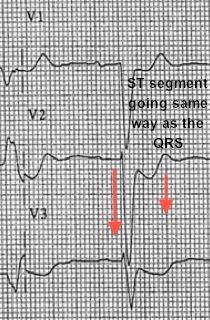
NB Dr Smith’s ECG has some great stuff on this here.
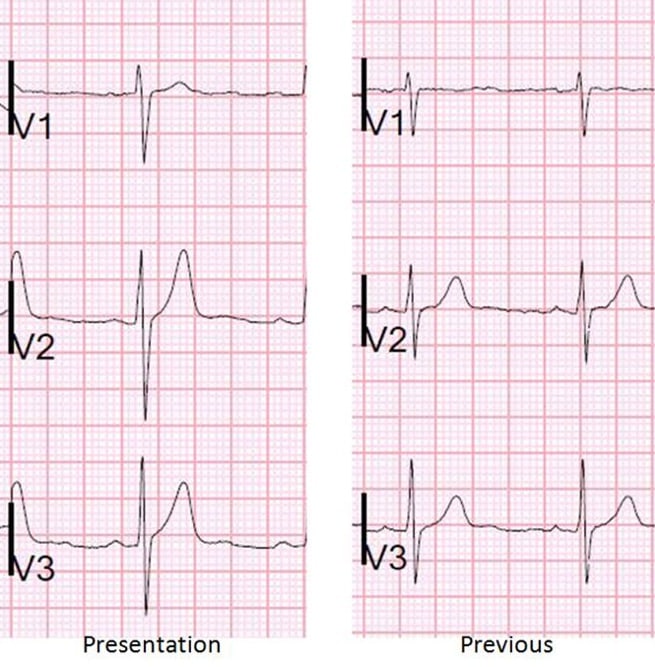
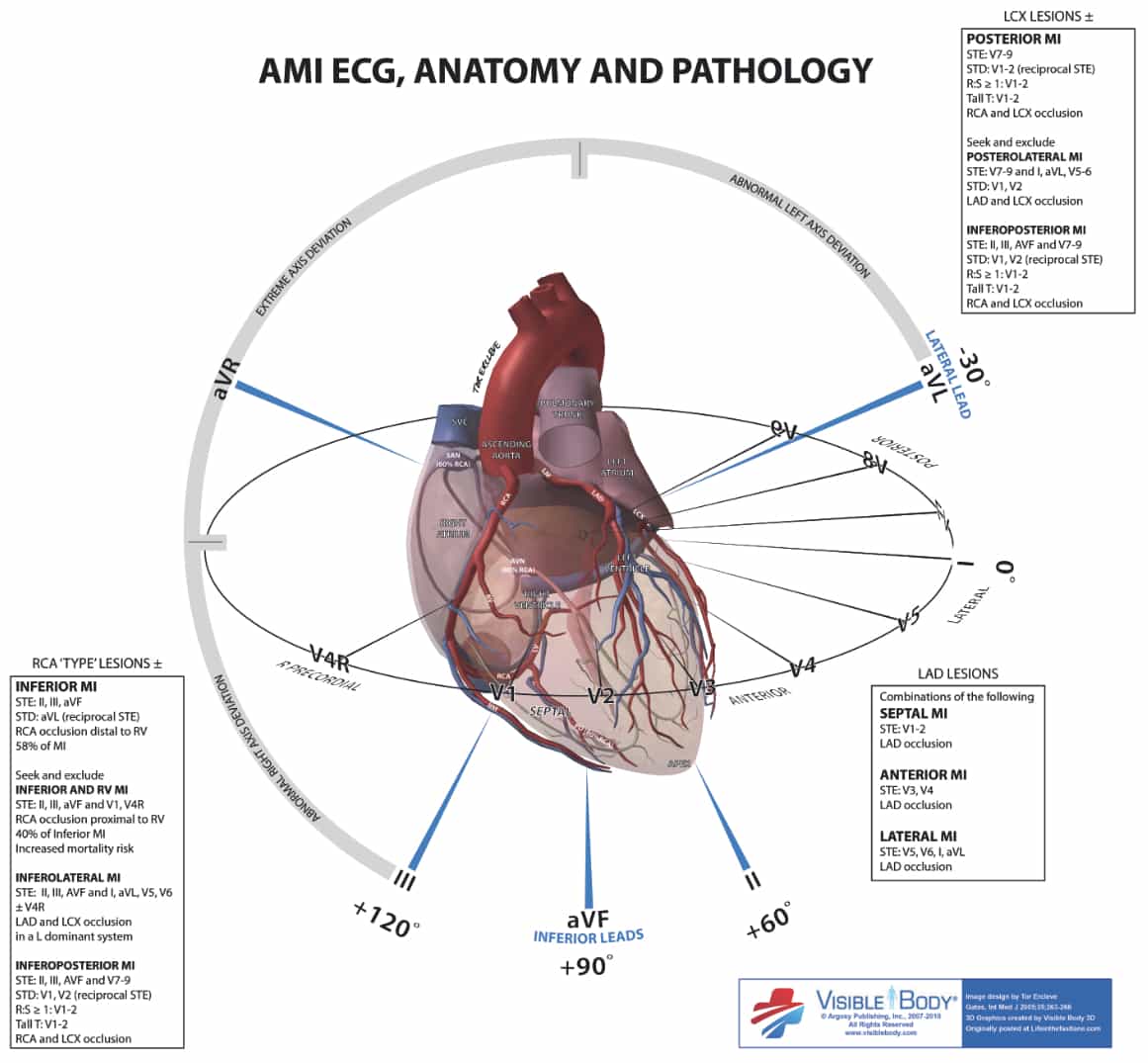
Posterior MI
- I’ve only picked this up more recently as I’ve got into ECGs a bit more
- this is the one where you’ve got ST dep anteriorly (V1-3) which is what post ST elevation will look like from the front.
- placing leads posteriorly will help confirm it. Though note the ST deviation will be smaller than seen anteriorly as the heart is an anteriorly placed structure in the chest and post leads are fairly far away from the post wall of the heart
- to confuse matters technically it’s not even the post wall that’s infarcting
- to confuse matters even further the nomenclature of naming the heart is a mess to start with…
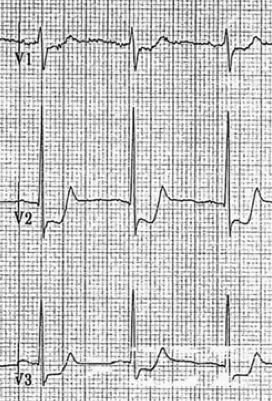
NB LITFL have a much more useful of delineating vectors and all that:
Left main coronary artery occlusion
- the first time I ever saw a talk by Amal Mattu he was going on about how “aVR don’t get no respect…” and it has of course stuck with me. ST elevation in aVR especially when associated with ST depression elsewhere should make you think LMCO
- if you are thinking that then the patient is lucky to have survived to hospital at all and may well not leave unless he gets a CABG.

De Winter ST/T wave complex
- this was completely new to me and to be honest looks a bit subtle for me to pick up
- 1mm ST up -sloping depression in V1-6 and peaked T waves
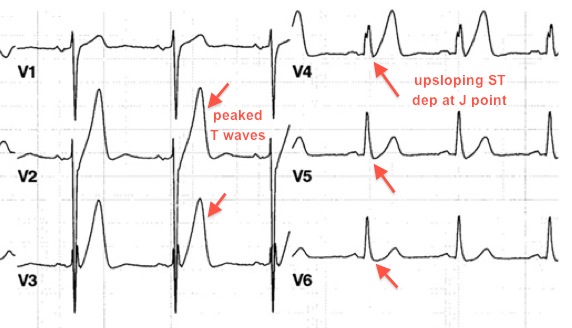
- Worth noting that this is quite different from Wellen’s (which most of you will know about) in two ways
- as it looks quite different
- represents a severe chronic LAD stenosis and not an acute occlusion
- the original ‘paper’ describing this is a simple letter to the editor in the NEJM, describing a case series
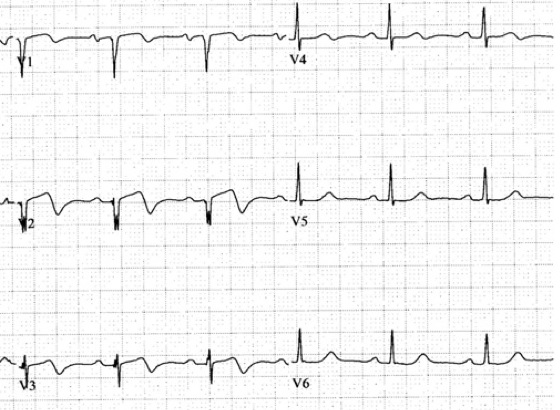
Hyper-acute T-waves
- this I picked up mainly from Dr Smith’s blog again. In particular with reference to BER and hyperacute T waves and prolonged QT suggesting ischemia not BER
- there are no examples from the paper but Dr Smith has a great example

Very much liked this review.
Thanks.
Very good article.
very much like this recent advancement in ekg interpretation.Amal Mattu doing a great job…