I’m back at the European Society for Emergency Meeting for another couple of talks (older ones can be found here , here and here…).
The slide is pinched from Dr Strangelove (via Chris Nickson…)
We all love to hate PE. We can’t seem to stop discussing it or publishing papers on it and there’s even a whole conference just on VTE. We have a similar love hate relationship with the dimer. It’s useful to use when it’s negative (cause we already knew the patient didn’t have a PE…) but it gives us sweats when it’s falsely positive on the patient with minimal symptoms who we never should have ordered it on in the first place.
We are in a position where we know we are both underdiagnosing PE in certain patients and overdiagnosing it in lots of others.
There are 2 new diagnostic strategies available to us.

One involves adjusting the normal level of d dimer based on age and the other modifies the dimer cut off based on clinical probability.
Both strategies apply to the low/intermediate risk patients. High risk patients should be going straight to CT and shocked/hypotensive patients should be trying to get to CT if you can make it and considering lysis. We do OK with this population already and let’s face it they’re not that common.
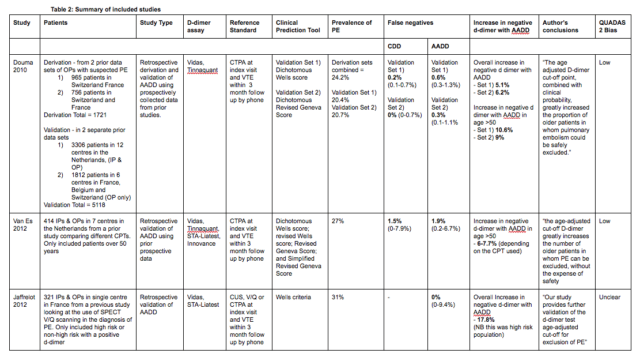
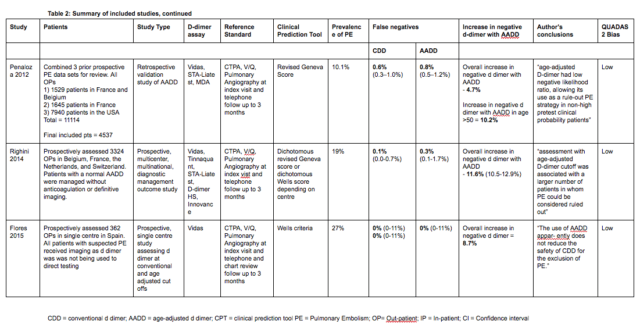
This has been around for a while. I did my CTR for the FRCEM on the topic. The data is all observational and of variable quality
The Righini paper is the big one here.
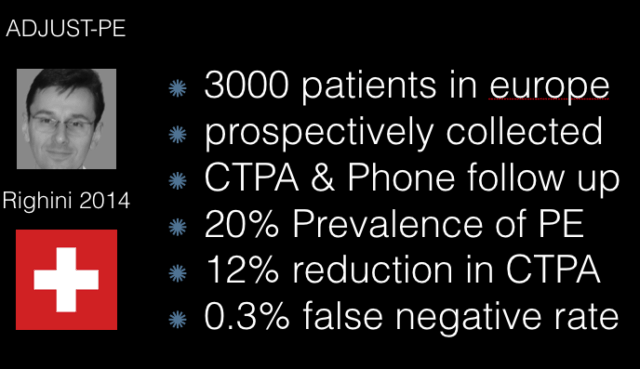
There is of course a false negative rate – you will miss a very occasional patient by using this strategy. however you will also miss PE with using a convention strategy. In the Righini paper it was 0.1 v 0.3
The major limitation here is that it only applies to the over 50s if you’re 35 your cut off is still 500 in this protocol. if you’re 85 then your cut off is 850 but it’s hard to see the downside of doing a CT on an 85 year old. The contrast nephropathy probably is non existent and the chance of serious pathology (PE or otherwise) is so much higher in this group.
So at its most basic the AADD reduces testing in people who i’m not in a rush to reduce testing in.
It has recently been endorsed by ACEP in their updated VTE policy so you now have a guideline to back you up (it is not as yet endorsed by ACCP or the ESC guidelines)
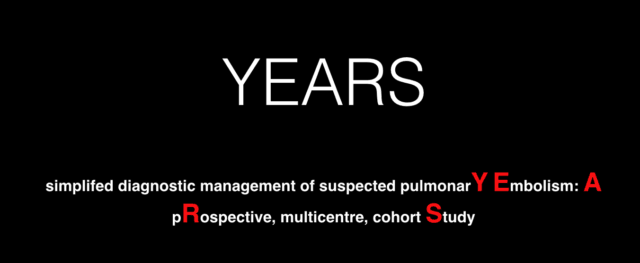
All studies seem to make some horrifically forced acronym out of the title. (PARAMEDIC2 is a good example…) This one is apparently the YEARS study. Though I didn’t see them even make any attempt to explain where the YEARS came from. I suggested this…
They modify the Wells criteria to just 3 questions.
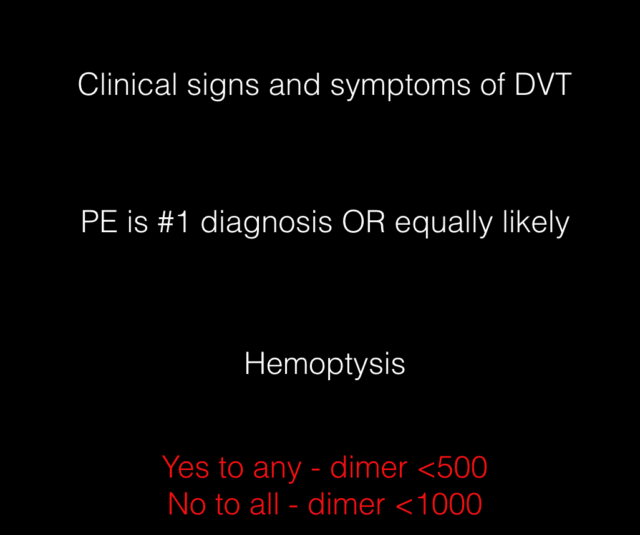
Your d dimer cut off is therefore dependant on your clinical risk.
My big concern with this paper is that the d dimer was done at triage before the assessing doctor answered the 3 questions. You can imagine that knowing the result of the dimer might change how you assign your pre test probability. Say you have a young female with a dimer of 950 and score negative on the other 2 questions of the YEARS protocol. The question “Is PE the most likely diagnosis” could be easily swayed by that knowledge.
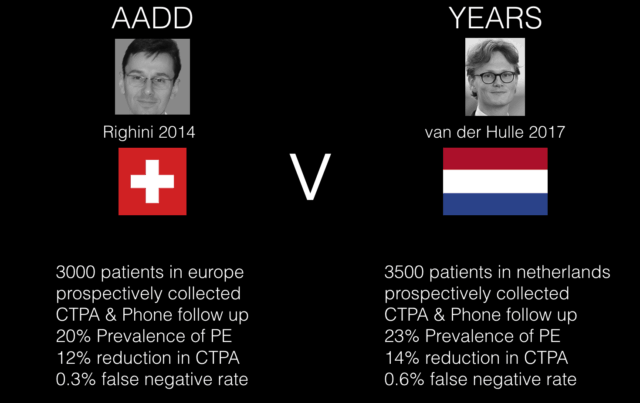
Honestly i think either are reasonable to use, certainly as part of a departmental protocol you’d be well supported. I think they’re both similar in terms of their evidence base and they both provide safe and modest reductions in current imaging levels.
This is an obvious question and the age adjusted dimer is jsut starting to be studied for this. So far it seems the reduction in imaging is even more modest and given the limited harm in just doing it yourself or getting a formal ultrasound then I can’t see it being great benefit.
Douma RA, le Gal G, Sohne M, Righini M, Kamphuisen PW, Perrier A, et al. Potential of an age adjusted D-dimer cut-off value to improve the exclusion of pulmonary embolism in older patients: a retrospective analysis of three large cohorts. BMJ (Clinical research ed). 2010 Mar 30;340(mar30 3):c1475–5.
Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. American College of Physicians; 2011 Oct 17;155(8):529–36.
van Es J, Mos I, Douma R, Erkens P, Durian M, Nizet T, et al. The combination of four different clinical decision rules and an age-adjusted D-dimer cut-off increases the number of patients in whom acute pulmonary embolism can safely be excluded. Thromb Haemost. 2012;107(1):167–71.
Jaffrelot M, Le Ven F, Le Roux P-Y, Tissot V, Rame E, Salaun P-Y, et al. External validation of a D-dimer age-adjusted cut-off for the exclusion of pulmonary embolism. Thromb Haemost. Schattauer Publishers; 2012 Apr 30;107(5):1005–7.
Penaloza A, Roy PM, KLINE J, Verschuren F, le Gal G, Quentin-Georget S, et al. Performance of age-adjusted D-dimer cut-off to rule out pulmonary embolism. Journal of Thrombosis and Haemostasis. 2012 Jul 3;10(7):1291–6.
Schouten HJ, Geersing GJ, Koek HL, Zuithoff NPA, Janssen KJM, Douma RA, et al. Diagnostic accuracy of conventional or age adjusted D-dimer cut-off values in older patients with suspected venous thromboembolism: systematic review and meta-analysis. BMJ (Clinical research ed). 2013 May 3;346(may03 1):f2492–2.
Righini M, Van Es J, Exter Den PL, Roy P-M, Verschuren F, Ghuysen A, et al. Age-Adjusted D-Dimer Cutoff Levels to Rule Out Pulmonary Embolism. JAMA. 2014 Mar 19;311(11):1117.
Jaconelli T, Crane S. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 2: Should we use an age adjusted D-dimer threshold in managing low risk patients with suspected pulmonary embolism? Emergency Medicine Journal. BMJ Publishing Group Ltd and the British Association for Accident & Emergency Medicine; 2015 Apr;32(4):335–7.
Flores J, de Tena JG, Galipienzo J, García-Avello Á, Pérez-Rodríguez E, Tortuero JI, et al. Clinical usefulness and safety of an age-adjusted D-dimer cutoff levels to exclude pulmonary embolism: a retrospective analysis. Internal and Emergency Medicine. Springer Milan; 2015 Sep 2;11(1):69–75.
Han C, Zhao Y, Cheng W, Yang J, Yuan J, Zheng Y, et al. The performance of age-adjusted D-dimer cut-off in Chinese outpatients with suspected venous thromboembolism. Thrombosis Research. Elsevier Ltd; 2015 Oct 1;136(4):739–43.
Crawford F, Andras A, Welch K, Sheares K, Keeling D, Chappell FM. D-dimer test for excluding the diagnosis of pulmonary embolism. Cochrane Database Syst Rev. 2016 Aug 5;(8):CD010864.
Takach Lapner S, Julian JA, Linkins LA, Bates SM, Kearon C. Questioning the use of an age-adjusted D-dimer threshold to exclude venous thromboembolism: analysis of individual patient data from two diagnostic studies. J Thromb Haemost. 2016 Aug 31;14(10):1953–9.
Monks D, Neill A, D B, Moughty A, A M, Timmons A, et al. Age Adjusted D-Dimer for exclusion of Pulmonary Embolism: a retrospective cohort study. Irish Medical Journal. 2017 Aug 9;110(7):1–6.
Riva N, Camporese G, Iotti M, Bucherini E, Righini M, Kamphuisen PW, et al. Age-adjusted D-dimer to rule out deep vein thrombosis: findings from the PALLADIO algorithm. J Thromb Haemost. 2017 Dec 8;16(2):271–8.
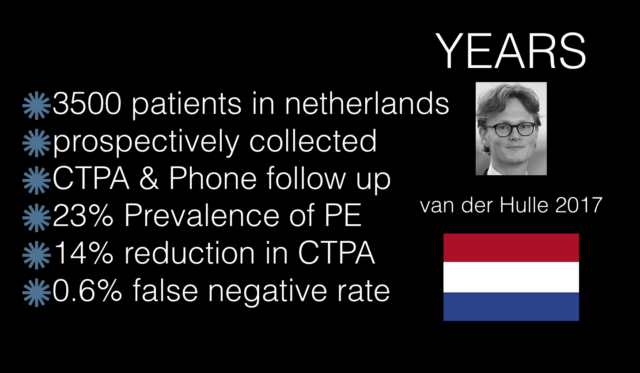
van der Hulle MD T, MD WYC, MD SK, MD LFMB, van Bemmel MD T, van Es MD J, et al. Simplifed diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study. The Lancet. Elsevier Ltd; 2017 May 22;:1–9.
Kabrhel C, Van Hylckama Vlieg A, Muzikanski A, Singer A, Fermann GJ, Francis S, et al. Multicenter Evaluation of the YEARSCriteria in Emergency Department Patients Evaluated for Pulmonary Embolism. Academic Emergency Medicine. Wiley/Blackwell (10.1111); 2018 Mar 31;:acem.13417–20.
RCEM Learning: Andy Neill & Dan Horner

Pingback: St.Emlyn's at #EuSEM18 - Day 2 - St.Emlyn's