From the wonderful Roberts & Hedges
Raised ICP
- normally ICP can rise to 80-100mmHg just when coughing/straining
- being intracranial hypertension has a huge list of associated conditions so just cause you’ve got headache, normal CT and a raised pressure on LP doesn’t mean you’re done with the diagnosis
- CSF is produced at 500 ml/day with a total of 150 ml in the system. This means there’s continuous circulation reabsorption. See the video for more details
[wpvideo Pzv6LzQp]
- the two types of hydrocephalus are:
- obstructive – expect big lateral ventricles and normal 4th as there’s a blockage somewhere
- communicating – general big ventricles but all the piping is OK, it’s the filter/drain that’s blocked – think blood pluggin the arachnoid villi
- one of the earliest clinical signs of raised ICP is reduced venous pulsation on fundoscopy – good luck with that…
- the old hyperventilation to reduce pCO2 and reduce ICP is a bit dodgy as it also does exactly what you don’t want it to do – it reduces cerebral blood flow.
- mannitol has two actions
- volume expander
- osmotic diuretic
- if osmolality is already >320 then mannitol won’t work.
- steroids work for vasogenic oedema from tumours but not anything else.
- paracetamol is effective for fever – this was news to me as I thought the fever was very much “cerebral” and not due to normal pathways
Intracranial shunts
- frequently put in for any long standing high ICP
- headache, nausea, vomiting, visual disturbance – think shunt malfunction
- failure of upward gaze an apparently sensitive sign
- there are a whole bunch of shunts available, both in terms of design and function. Here’s a video of how to place one:
[youtube=http://www.youtube.com/watch?v=ptbG5m7MBE8&w=640&h=360]
- even more interesting, here’s a wonderful paper (free) of lots of different types of devices you might find in the head and neck, shunts included.
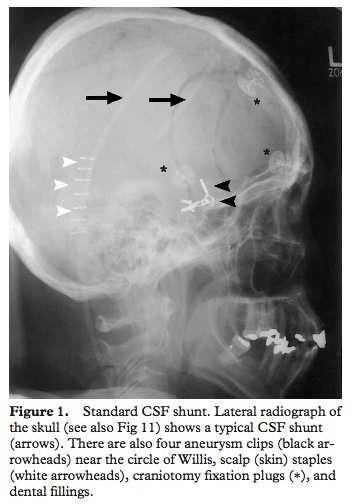
- shunts are normally placed in the anterior horn of the right lateral ventricle as this is non-dominant for most people so any damage caused will hopefully be less significant
- there are lots of reasons for malfunction
- blood or debris in the proximal site (choroid plexus within the ventricle can get stuck in it
- fracture of the tubing along its course
- infection of the tubing along its course
- something like a piece of omentum getting stuck in the distal port in the abdomen
- there are characteristics of “valve pumping” that might tell you where the obstruction is but apparently they’re only present 5% of the time so i’ll not bother you with the details.
- the valve looks like this:
- when you press on it normal refill time should be about 15-30 secs. I have no where near enough experience to be able to press on these and have any ideas what it means. Anyone else have any thoughts on whether this is useful?
- with sterile technique you can access it for CSF. Be sure and use a small needle and approach it at a shallow angle (about 30 degrees or so) rather than coming at it perpendicular to the skull. Apparently this reduces damage to the valve.
- CT scan has sensitivity of 80% and shunt series (plain films of neck and abdo) has sens of 20% but you still need both. Obstruction isn’t a simple yes/no diagnosis a lot of the time and you need old CTs to compare with

