I’m entering a few months prep for the UK and Ireland exit exam in Emergency Medicine: the FRCEM. I’ll be adding lots of little notes on pearls I’ve learned along the way. A lot of my revision is based around the Handbook of EM as a curriculum guide and review of contemporary, mainly UK guidelines. I also focus on the areas that I’m a bit sketchy on. With that in mind I hope they’re useful.
You can find more things on the FRCEM on this site here.
Some useful RCEM Guidance in the silver book with a nice page from the RCEM Learning site too. RCEM have also published an audit on care of older persons
NICE 2010 has it’s own guidance
(this is NICE 2010, but they all contain the same 3 components)
Delirium (sometimes called ‘acute confusional state’) is a common clinical syndrome characterised by disturbed consciousness, cognitive function or perception, which has an acute onset and fluctuating course.
- change in consciousness (hyperactive, hypoactive)
- impairment of cognition, memory or attention
- acute/fluctuating course
- sepsis
- low or high sugars
- CNS infections
- psychiatric illness
- alcohol, both intoxication and withdrawal
- drugs
- almost all
- anti cholinergics common
- thyroid issues
- hypoxia
- pain
- sodiums and calciums
- uraemia
- liver failure
- and lots of others…
- age>65
- cognitive impairment
- hip fracture
- severe illness
- The Confusion Assessment Method is in NICE 2010 and on the current RCEM curriculum
- 1) acute onset or fluctuating course
- what it says on the tin
- 2) inattention
- classically a “poor historian” or difficulty recalling months of years backward
- 3) disorganised thinking
- incoherent, rambling or irrelevant speech
- basically Trump on a good day…
- 4) altered level of consciousness
- from agitated restless to somnolent
- 1) acute onset or fluctuating course
- there is a CAM ICU version for the sicker folk
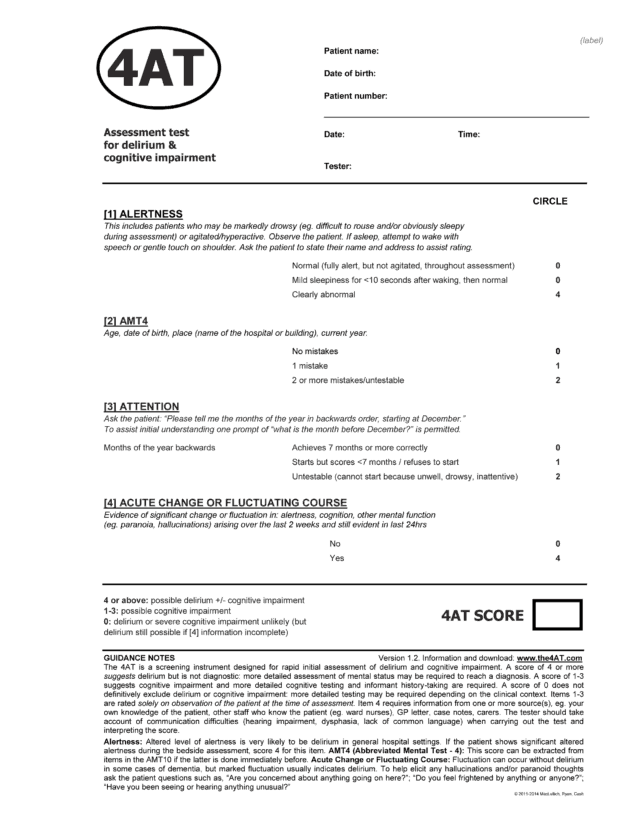
- the 4AT is another potential screen
NICE 2010
- staff familiar to the patient
- don’t move room or ward
- involve a tailored multi disciplinary intervention within 24 hrs
Some general points
- reorient patients frequently
- clocks with a clear day and date
- cognitively stimulate (ask them about their family or the old days or try a twiddle muff…)
- facilitate visits
- physical areas in ED should be visually and acoustically separate which are well lit and well sign posted
- non skid floor
- hand rails
In terms of medicating agitation
- usual non pharmacological stuff first
- NICE recommends haloperidol or olanzapine for a short course
- remember to avoid in Parkinson’s
nicely summarised in the executive summary of the silver book
older persons typically (not rarely) present with non specific syndromes rather than the classic presentations in younger people
- Falls
- syncopal
- non syncopal eg vestiubular, strength, balance etc
- Immobility
- anything from progressive dementia to cord compression
- Delirium and dementia
- dlirium can have varying degress of consciousness
- Delirium and dementia are distinct and have different management
- Polypharmacy
- many presentations can involve meds
- consider STOPP/START as a way of screening the meds
- Incontinence
- marker of frailty
- main problem is mis labelling it as a simple UTI based on dipstick testing
