I’m entering a few months prep for the UK and Ireland exit exam in Emergency Medicine: the FRCEM. I’ll be adding lots of little notes on pearls I’ve learned along the way. A lot of my revision is based around the Handbook of EM as a curriculum guide and review of contemporary, mainly UK guidelines. I also focus on the areas that I’m a bit sketchy on. With that in mind I hope they’re useful.
You can find more things on the FRCEM on this site here.
I’ve never used digibind since i was an intern (and that was literally me attaching it as someone else ordered it). It’s one of the ones that is very testable that I don’t know much about.
From Toxbase, OHEM 4th and Rosen’s 8th
How does digoxin work?
- increases myocardial contratility by blocking N-K-ATPase, increasing extracellular potassium and ultimately increasing the amount of calcium put into the sarcoplasmic reticulum causing increased contraction
- slows rate by blocking AV node (can also increase vagal output and reduce SA activity)
- half life is 30-40 hours and can be severely prolonged in renal impairment
[collapse]
What types of toxicity are there and how do they present?
- acute
- either in someone naive to the medication or on it long term
- nausea, anorexia, fatigue, visual disturbance (all very vague)
- new arrhythmias is the big thing to look for
- chronic
- this is much more insidious with a higher mortality possibly related to the underlying comorbidities
- dig levels
- steady state concentrations predict toxicity rather than peak (usually around 6-8 hours post acute OD)
- levels are particularly tricky in chronic toxicity were lowish levels of 2-6 can still be associated with mortality
[collapse]
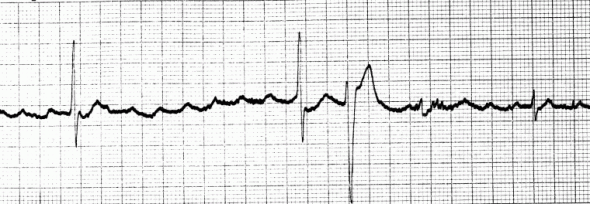
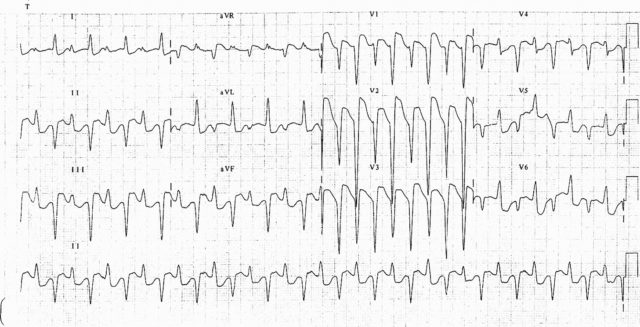
What are the ECG changes?
How is it managed?
- there are 2 antidotes
- DigiBind/DigiFab (different brands as far as i can work out, DigiBind has been discontinued)
- Digoxin Fragment antigen-binding antibodies
- Indications (as per Toxbase)
- severe brady or ventricular arrhythmias
- hyperkalaemia
- Dosing
- this is complex but well described on Toxbase with some subtleties regarding full and partial neutralisation. I’m never gonna remember that for the exam so I’m not putting it here.
- Rosen’s has empiric 10 vials in an acute severe OD, with 20 in cardiac arrest.
- Traditionally people have talked about avoiding calcium for the hyper K given the mysterious “stone heart syndrome”. This is probably not a big risk and Toxbase agrees saying it’s fine to give the calcium
- there is some enterorhepatic recirculation so this is one of the times to “consider” multi dose charcoal
[collapse]