This is no small topic. And I don’t plan to give a definitive take on this but here’s some thoughts.
I’m also planning one on why methaemoglobinaemia is a good thing. Seriously.
[peekaboo_link name=”1 What is methaemoglobinaemia?”]1 What is methaemoglobinaemia?[/peekaboo_link]
[peekaboo_content name=”1 What is methaemoglobinaemia?”]
Iron is normally found in Hb in the ferrous (Fe2+) state. In metHb the iron is in the ferric (Fe3+) state.
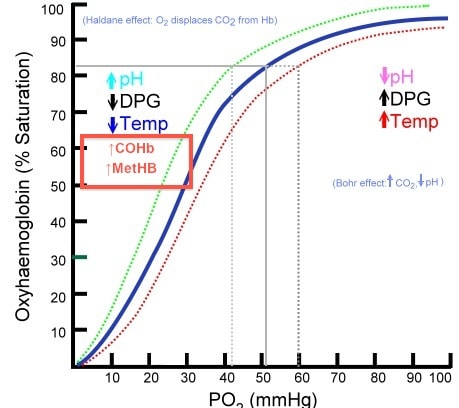
MetHb is unable to bind oxygen and any nomral Hb left will have greater affinity for the O2 and not want to give it up. Together this shifts the good old oxy-Hb dissociation curve to the left (as does carboxyhaemoglobin)
 The important clinical effect of this is tissue hypoxia.
The important clinical effect of this is tissue hypoxia.
Note this is importantly different from cyanide toxicity, where the interruption is in the electron transport chain and oxygen transport is unaffected.
[/peekaboo_content]
[peekaboo_link name=”2 Causes”]2 Causes[/peekaboo_link]
[peekaboo_content name=”2 Causes”]
- congenital – we’ll not worry too much about these
- acquired
- iatrogenic – the big one we should be aware of LA toxicity (notably prilocaine, and though rarely used I have seen this). The other notable one is metoclopramide which was new to me… Dapsone is another but when did you last see someone on dapsone? [UPDATE 2015 – just recently saw a dapsone OD, multiple doses of blue over a few days…]
- poisoning – the nitrites (amyl nitrite or sodium nitrite). Doses as small as 3 or 4g are known to be fatal for an adult. Of note sodium nitrite is widely used in food preservation and appears and tastes like normal salt. So imagine the potential for problems there. See this report for an example. In industrial settings it is often highly coloured to make it conspicuous.
[/peekaboo_content]
[peekaboo_link name=”3 Clinical Features?”]3 Clinical Features?[/peekaboo_link]
[peekaboo_content name=”3 Clinical Features?”]
Hopefully you know the general effects of tissue hypoxia – it makes you sick, potentially very sick.
The more useful clinical features are probably:
- blueish skin colour – naturally bog-standard hypoxemia will cause this but there is more of a blueish tinge to it. Note the blue men of Lurgan who were a famous case series of congenital metHb. Lurgan is a whole 5 minutes away from where I grew up and where I practice. Just saying…
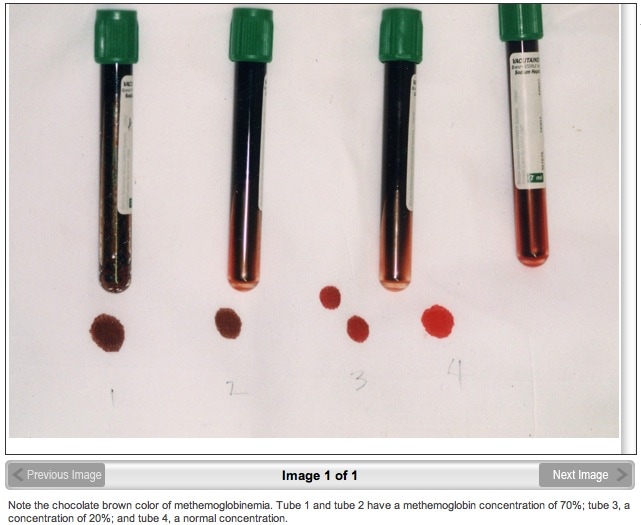
- chocolate brown discoloration of the blood. In one of the cases I’ve seen it was a lot more dramatic than the colour shown below
- plays silly buggers with your SaO2 readings – as i’m sure you all know (ahem…) that standard sats probes emit only two wavelengths (650nm and 940nm) that correspond to the absorption of oxy- and deoxy- haemoglobin. MetHb absorbs at yet a different wavelength and so is not picked up usually on basic monitoring. The same is true of COHb. You can get sats probes that measure different wavelengths but that’s a whole different discussion…
- also worth considering if your sats don’t get better despite O2
[/peekaboo_content]
[peekaboo_link name=”4 How do you make the diagnosis?”]4 How do you make the diagnosis?[/peekaboo_link]
[peekaboo_content name=”4 How do you make the diagnosis?”]
- a history of exposure to something that might cause it
- a raised MetHb level – most blood gas machines will measure this (if they have a thing called a co-oximeter). If your machine lists COHb levels then it’ll probably give you MetHb levels too. A level above 20% is often quoted to stimulate treatment
[/peekaboo_content]
[peekaboo_link name=”5 Treatment?”]5 Treatment?[/peekaboo_link]
[peekaboo_content name=”5 Treatment?”]
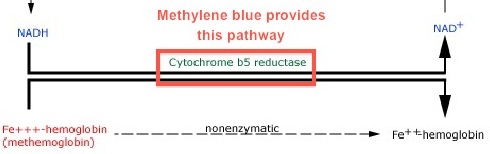
- methylene blue – you remember that funny dye from high school chemistry? and remember that cupboard in your ED that has all the antidotes that you can’t pronounce in it? – it’ll be in there.
- 1-2 mg/kg IV over 5 minutes, response should be “rapid”
- doses can be repeated but there’s reports of badness beyond 7 mg/kg
- note that UpToDate suggests that methylene blue is measured as MetHb in standard co-oximeter readings so I doubt that you can use MetHb to judge clinical response. Anyone know any better on this? I couldn’t find much.
- I’m presuming you’re all find with good supportive care like airway and fluids and all that
[/peekaboo_content]
[peekaboo_link name=”6 How Does Methylene Blue Work?”]6 How Does Methylene Blue Work?[/peekaboo_link]
[peekaboo_content name=”6 How Does Methylene Blue Work?”]
[/peekaboo_content]
[peekaboo_link name=”7 Some observations”]7 Some observations[/peekaboo_link]
[peekaboo_content name=”7 Some observations”]
This is rare stuff, lets face it. I’ve seen a grand total of one severe poisoning from this. But to be perfectly honest if we don’t know this stuff, then no one else in the hospital will. And remember – people won’t always tell you about drug exposures so you have to be able to put the diagnosis together in the absence of information. After all that’s what we do right?
UPDATE
Matthew Mac Partlin added a few comments with some good bits that were useful to me at least!
- deoxygenated blood reds up nicely when exposed to air, but Met-Hb blood keeps its chocolatey colour.
- Watch that SpO2 when you give the methylene blue! It usually takes a spectacular dive as the ferrous-Hb is released.
[/peekaboo_content]
References:
- Occupational methaemoglobinaemia. Mechanisms of production, features, diagnosis and management including the use of methylene blue. Bradberry SM Toxicol Rev. 2003;22(1):13-27. PMID 14579544
- UpToDate.com
- Toxicology Handbook 2nd Ed Murray et al Churchill Livingstone 2011
- Wikipedia – though beware what you find there…


I’ve seen one case of it. Took care of him in the ICU. Diagnosed by one of my stellar third year residents in the ED, got methylene blue, and then had undiagnosed G6PD deficiency, and started hemolyzing. Very very sick.
We frequently talk about “you give a blue drug to a blue patient and they turn red,” but our blue patient got a blue drug and turned him red, then turned him white (anemia), and then turned him yellow (hyperbilirubinemia).
all the colours of the rainbow!
Actually I have a patient on Dapsone! For dermatitis herpetiformis not leprosy!
Fair point peter! Though I suppose that won’t land them up with us hopefully!
Pingback: Why methaemoglobinaemia is a good thing | Emergency Medicine Ireland
Thank you for your informative site. My brother before me died at 1 month from methaemoglobulin anemia from the nitrates in the well water in Southern Alberta. Canada. on the farm They had no idea at the time of the cause (circa 1950) I was born in 51
and was breast fed..probably saved my life. The DR at the time thought i was blue as I was born breach with umbilical cord double wrapped on neck. I am 61
and the symptoms have been managable…..it is a good thing because though I have had to fight like hell to keep on the weight or stay warm….I am a thinner person thereby not having to deal with many of the side effects of FAT. And I do love my potatoes . CL
Hi I have this and cant find anyone who has it and I need help to found out how I live with this you
Two quickies –
1) I saw 3 cases over 3 years (I work in Australia). The first 2 were an asian couple who had imported Chinese meat product containing a boric acid & nitrite compound. The second was a young soldier who had been on chloroquine for malarial prophylaxis. Apparently recluse spider bites can do it too (Not likely to be a big threat in Ireland)
2) The diagnostic clue pattern is a combination of a cyanosed patient who usually doesn’t feel too bad and has a low SpO2 with a fairly normal PaO2 and whose cyanosis and SpO2 fail to improve with increased FiO2. Also, deoxygenated blood reds up nicely when exposed to air, but Met-Hb blood keeps its chocolatey colour.
Watch that SpO2 when you give the methylene blue! It usually takes a spectacular dive as the ferrous-Hb is released.
Great comments I’ll try and add them to the post
Andy Neill http://EmergencyMedicineIreland.com
Is there anyway to find out if this exhists up your bloodline? Are there any studies currently being conducted of the long term effects on bloodlines or future generations?
Hi Joni
Afraid I don’t know the answer to your questions. Sorry.
Andy
Thank you so much for your timely reaponse!