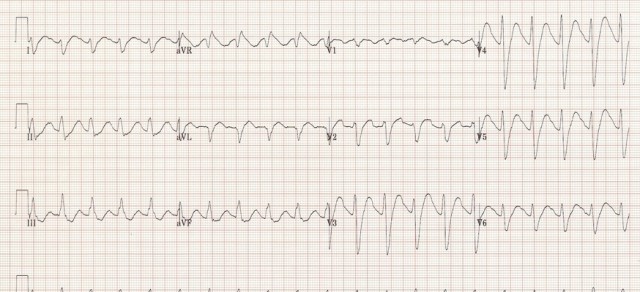
The ECG in the poisoned patient
Most patients presenting to the ED with either accidental or intentional drug ingestion will get an ECG. In most departments I’ve worked in, the senior doctor looks at all the ECGs, primarily for STEMI, but for other findings too. The … Read More »