Tasty Morsels of EM 039 BradyDysrhythmias
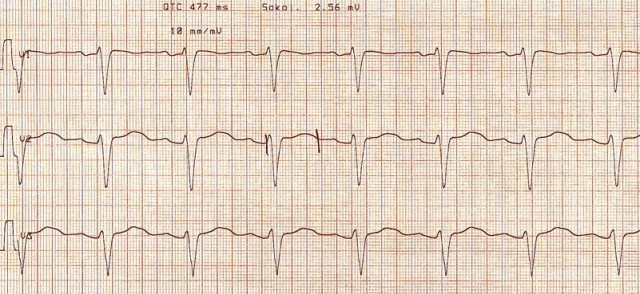
[Featured image via LITFL] Approach to BradyDysrhythmias EB Medicine Article [free via EMRA if you’re a member. About 70 dollars a year. Well worth it.] On a FOAMed note, it’s interesting that all the ECGs in the article are … Read More »