Though I suspect this is old news by now, I’ve just read a couple of papers on it and thought I’d share my thoughts. They’re both by the very smart and talented Kenji Inaba.
Question
- where should we put a cannula if we want to decompress a tension pneumothorax?
Inaba, Kenji, Bernardino C Branco, Marc Eckstein, David V Shatz, Matthew J Martin, Donald J Green, Thomas T Noguchi, and Demetrios Demetriades. “Optimal Positioning for Emergent Needle Thoracostomy: a Cadaver-Based Study.” The Journal of Trauma: Injury, Infection, and Critical Care 71, no. 5: 1099–1103. PMID 22071914
METHODS
- 20 fresh frozen cadavers
- 14G 5cm cannulae placed in 2nd ICS and 5th ICS
- throacotomy to assess pleural puncture (considered a +ve outcome)
- chest wall thickness measured in each cadaver at each puncture position
RESULTS
- total of 80 punctures
- all succeeded in the 5th ICS; 57% succeeded in the 2nd ICS
BOTTOM LINE
- stick it in the 5th ICS [if at all]
—
Inaba, Kenji, Crystal Ives, Kelsey McClure, Bernardino C Branco, Marc Eckstein, David Shatz, Matthew J Martin, Sravanthi Reddy, and Demetrios Demetriades. “Radiologic Evaluation of Alternative Sites for Needle Decompression of Tension Pneumothorax..” Archives of Surgery (Chicago, Ill. : 1960) 147, no. 9: 813–818. PMID 22987168
METHODS
- chart and image review of all their trauma pts over a year who got a chest CT
- split them into BMI quintiles
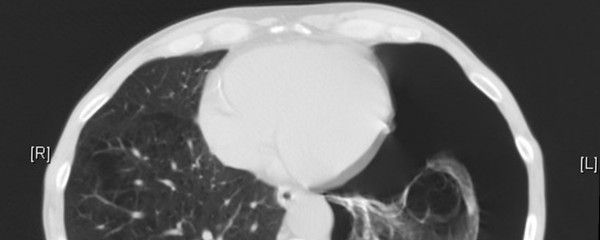
- measured the chest wall thickness on CT at the 2nd ICS and 5th ICS
RESULTS
- 680 pts
- 46mm in the 2nd ICS; 33mm in the 5th ICS
- half of the pts had a chest thicker than 50mm at the 2nd ICS
BOTTOM LINE
- if a standard 14 G cannula is 50 mm then we’re going to fail to drain a whole bunch in the 2nd ICS
—
MY THOUGHTS
I’ve drained a number of tension PTX in the past – it’s usually fun to get the hiss – all have been in the ED and quickly followed by a chest drain. I’ve received a number from the pre-hospital environment that probably worked initially but now the cannula has kinked and a second cannula shows a second release of air.
All this is a little bit silly I think – as I’m now convinced that we just need to get on and do the bloody drain (or at least make a cut and stick a finger in). If the patient is crashing in front of you and the quickest option is to place a cannula then great – just don’t get lulled into thinking you’ve fixed the problem.
UPDATE:
Haldun Akoglu left a comment about a paper that he just published (PMID 23116647). It was a review of 150 CT scans of people with PTX, mainly traumatic. They found that a 5cm cannula would also fail a lot of the time but failed to find a thinner chest wall at the 5th ICS when compared with the 2nd. I’m not sure why they they didn’t find a difference when Inaba did but either way 5cm cannulas are not the way to go.

What about 3.25 inch (8.25 cm) catheters? North Carolina has standardized on a minimum of 14ga 3.25 inch for needle decompression of PTX.
I think 8.25cm would be a lot better at getting across the whole chest wall. I presume these are cannulas specifically for decompression, not IV access?
We use 8.25cm here in Tennessee and I’ve never had a problem, They seem to be used fluently in the radiology field.
I’d be pleased if u can check our recent research on this subject. I’d love to have your comments. Thanks. Injury. 2012 Oct 29. pii: S0020-1383(12)00455-X. doi: 10.1016/j.injury.2012.10.005. [Epub ahead of print]
Determination of the appropriate catheter length and place for needle thoracostomy by using computed tomography scans of pneumothorax patients.
http://www.ncbi.nlm.nih.gov/pubmed/23116647
cheers fot the link Haidun, will have a read at the paper.
Hi Andy. Can I ask? What line do you then use for the 5th ICS placement? Still MCL or AAL or MAL? Thanks for a great post once again!
according to the Inaba paper they talk about using the 5th ICS just anterior to the mid axillary line.
Great post Andy
Have seen many a pre-hospital pneumocath sitting in pec muscle. I was taught by a trauma guru in Melbourne that when dealing with tension pneumothorax, the goal is to “decompress the chest”, not “get the needle in”, nor “get the tube in”. Based on this, in a supine major trauma patient, if you have a scalpel & your blunt dissecting tool of choice on hand, just make the hole you plan to put your chest tube in. Faffing around with needles can – as you point out – actually waste time, fail, and then you go for the tube anyway. And to reiterate, don’t rush the tube. Once the chest is decompressed you can relax (a bit!)
If you do go for a needle, use the longest one you can. Never use a standard short IV-access IV. Use a longer (8-10 cm) IV, or, open your central line kit, and there’s a longer 16G IV in most that you can use, and I agree, go for the 5th.
i haven’t done this in a while but next time i plan to just make a cut and puncture a hole in the pleura. We all know we’re committed to a chest drain once we stick the needle in but i suspect we’re still a little hesitant.
Hi Andy,
Having recently performed bilateral finger thoracostomies during CPR on a patient with PEA arrest due to suspected tension pneumothorax, I can tell you that I wouldn’t go back to using a needle. Each side took 5-10 seconds, max, and even with someone jumping up and down on the chest it was pretty straightforward. In comparison, the pre-hospital 14g needle went straight through the apex of the lung and caused a massive haemothorax, which compounded an already desperate situation. When I put my finger in I could rapidly tell which lung was up and which one wasn’t, avoiding any further trauma to the lungs, and I used the same holes to put in bilateral chest drains. This experience convinced me that finger thoracostomy is safer and more efficient than needle thoracocentesis. The only place for a needle is if you don’t have a scalpel!
I’m still waiting for my chance to play with the scalpel instead of the needle but i agree entirely!
Great post and comments thanks Andy; Always good to see dogma challenged! 5th space anterior to MAL makes a lot of sense given that this is where the drain is going. I use this approach for aspirating spontaneous Pnthx too as can convert to drain in same way if required.
yeah, that’s my next step, i’ve still been aspirating through the 2nd (for simple spont PTC) but wondering if i should move to 5th. Less muscle mass = less pain?
There is a great review of pleural decompression techniques by Fitzgerald et al from The Alfred Hospital in Melbourne, published in Injury 2008, 39(1):9-20. (http://www.ncbi.nlm.nih.gov/pubmed/18164300)
Their findings include the following quote:
“1. Needle thoracocentesis is an unreliable means of decompressing the chest of an unstable patient and should only be used as a technique of last resort.
2. Blunt dissection and digital decompression through the pleura is the essential first step for pleural decompression, as decompression of the pleural space is a primary goal during reception of the haemodynamically unstable patient with a haemothorax or pneumothorax. Drainage and insertion of a chest tube is a secondary priority.”
Ed
Cheers for the link Ed – your comment got buried int he spam for a while there (might have been the hyperlink).
I obviously need to read the original paper when I get a hold of it, but is it muscle or fat or fat in the muscle that makes it difficult for a needle to work ?
Where was the study performed, what is the average “patient” weight or BMI ?
Maybe it depends. There are places in the world where obesity is less widespread than in others ?
i think it’s just the distance from skin to pleura that’s the problem. Whether it’s muscle or fat doesn’t seem to matter
Agree, finger thoracostomy is preferable. Challenge is for e non physician pre hospital provider. Do we continue to teach needle decompression and used a different cannula/position or just not bother because it is a relatively infrequent presentation and needle decompression is imperfect (but may work).
Good point – should we be giving scalpels to all the paramedics? Given how infrequent it must be for paramedics i suspect stick with the cannula
Agree.
Finger thoracostomy JUST for patients under positive pressure ventilation? Or for spont vent too. Can take a few mins to get chest drain set up…
http://www.ncbi.nlm.nih.gov/pubmed/24381693, We did a serial of not just ptx but all chest walls to get a random gague of how far off we would be, longer is better but a technique were you can aspirate air for success may be better
Pingback: Pneumothorax | thoracotomie
Pingback: We Don’t Know the Midclavicular Line | | HEMS Critical Care
H&H Medical has an Enhanced Pneumothorax Needle with a larger non collapsible stainless steel Cannulae — http://buyhandh.com
H&H Medical has an Enhanced Pneumothorax Needle with a larger non collapsible stainless steel Cannulae——————— buyHandH.com
Pingback: Chest Trauma – rathemblog
Gents, perhaps consider Thoraquick for Patamedics?
*Paramedics
I know a flight team that just used a scalpel and a blunt trocar with just a chest tube release to air for decompression. It was the same placement as a normal chest tube, 5th ICS MAL. Worked for both ptx and hemos. After the initial drain/release, clamp it off with a large hemostat clamp.