This should surely be kind of a big deal. Given that it seems to be evidence of something cheap, easy to give that seems to make (albeit) a difference in mortality outcomes without any signs of problems.
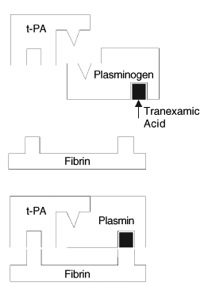
I had vague memories of tranexamic acid from O&G stuff but wasn’t even on my radar for trauma.
Let me try and summarise the paper
Methods
- the usual good stuff
- double blind, randomised all that jazz
- 20000 patients – yes that’s right 20000 patients…
- included patients with or “at risk of” (that’s the tricksy phrase) major bleeding from trauma
- outcome was death and subdivided according to cause
- Pfizer supplied the drug and placebo but nothing else that I can see
Results
- death 14.5% vs 16% favouring tranexamic acid over placebo
The always inconvenient and tricky details
the inclusion criteria are the real difficulty in this paper. You could get in if you had major bleeding (which seems to be defined as low BP and tachy) OR if someone felt you were at risk for bleeding. Let me quote a bit
Patients were included if the responsible doctor was substantially uncertain about whether or not to treat with tranexamic acid (ie, entry was governed by the uncertainty principle). Patients for whom the responsible doctor considered that there was a clear indication for tranexamic acid were not randomly assigned
- how do i know if i’m substantially uncertain?
- what are the clear indications for tranexamic acid – i presume that’s what this trial was to find out
Interpretation
the reason this trial was so big is that they were looking for a small improvement in mortality and that’s just what they found. It looks like a fairly easy way to get that improvement.
The problems in the inclusion criteria are real but it’s worth remembering that the way they set up the study will tend to include less sick patients and I would imagine that would reduce the observed treatment effect.
The other thing to remember is that we only expect tranexamic acid to reduce death from bleeding not the other causes so note that bleeding was only cause of death in about 1/3 of the patients who died. Again this should reduce not increase the treatment effect.
So in the sicker, truly bleeding patients (say with mortality rates of 50%) then you’d expect the improvement to be greater than 1.5%.
They had a 70/30 split between blunt and penetrating injury which is probably more than us but I have to say I found this fairly compelling
Any thoughts? Anybody used this yet?
For the ultimate brief-take on this check out the always excellent NNT

Pingback: The LITFL Review 020 - Life in the FastLane Medical Blog
Pingback: CASE #6 UPDATE – FIND THE BLEEDING, STOP THE BLEEDING « Rural Doctors Net
Pingback: Trauma! Massive Transfusion • LITFL • Trauma Tribulation
Pingback: Managing the Critical Bleeder!! • LITFL • Hematology Hoodwinker
Pingback: R&R in the FASTLANE 015 • LITFL