Seeing as my day job is meant to be anatomy I figure a few posts focused on anatomy with relevance to EM might be nice. For me at least.
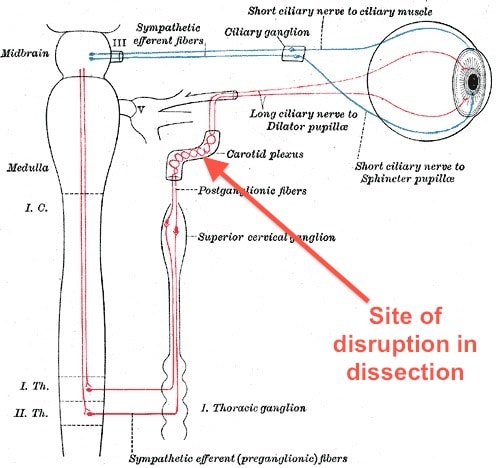
[Image from Nautiyal A, Singh S, DiSalle M, O’Sullivan J (2005) Painful Horner Syndrome as a Harbinger of Silent Carotid Dissection. PLoS Med 2(1): e19 doi:10.1371/journal.pmed.0020019 via Wikipedia Commons]
Horner’s syndrome in med school means
Never seen one.
Horner’s syndrome in the ED should mean
- some kind of dissection originating or extending to the carotids (spont or trauma)
- cavernous sinus thrombosis
Have seen one of each. And no doubt missed a bunch more!
We also hope the patient presents with pain, otherwise we’ll not bother looking for it.
So what is Horner’s syndrome?
Despite common assumptions it is not the result of impaling the thumb on a cooked piece of fruit but was named after this chap
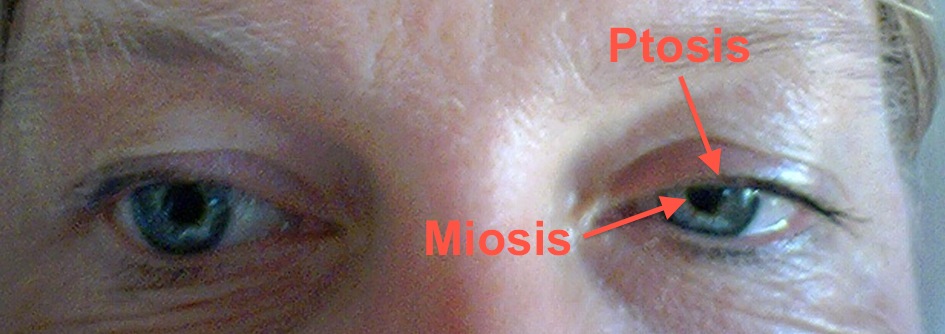
Consists of:
- miosis
- ptosis
- anhydrosis
can we simplify this?
- small pupil on the side of the lesion
- droopy lid on the side of the lesion
no one cares that your face doesn’t sweat so forget about it
Bottom line:
- The sympathetic supply to the eye has been disrupted
 [Image from Wikipedia Commons in the public domain. Note this diagram only shows the parasympathetic fibres passing through the ciliary ganglion. In reality both the sympathetic and parasympathetic fibres are thought to pass through the ciliary ganglion but only the parasympathetic fibres synapse]
[Image from Wikipedia Commons in the public domain. Note this diagram only shows the parasympathetic fibres passing through the ciliary ganglion. In reality both the sympathetic and parasympathetic fibres are thought to pass through the ciliary ganglion but only the parasympathetic fibres synapse]And what does the sympathetic nerve supply do?
- it supplies the dilator pupillae muscle (makes the pupil big)
- it supplies the fairly puny Muller’s muscle that helps keep the eyelid raised
Where does the disruption happen?
- Potentially this can be anywhere between brainstem and the eye but for our purpose we’re talking about a third-order lesion (if you can’t remember all that first, second order neurone thing then don’t worry too much) meaning the fibres from the sympathetic trunk to their final destination.
- These are carried as a plexus in the wall of the carotid artery. This is where they tend to get disrupted in any of the dissections or neck trauma.
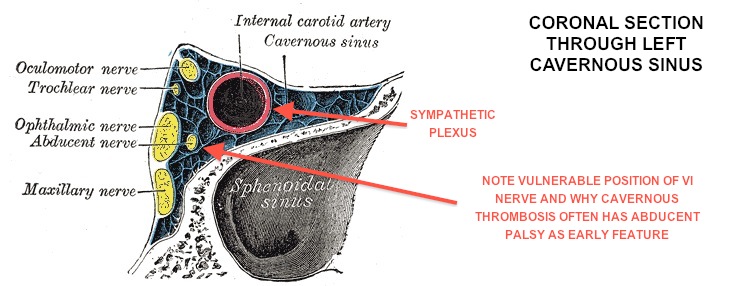
- The other spot we’re interested in is in the cavernous sinus itself. In that case you’ll be looking for ipsilateral funny eye movements as well as the Horners (probably the most useful sign)
[Image from Netter’s]
 [Image from Wikipedia Commons. Public Domain]
[Image from Wikipedia Commons. Public Domain]Key Pearls
- turn off the lights – tell your patient first. When the lights are off the pupils should dilate up. If there’s a Horner’s syndrome the normal pupil will get bigger and the affected one will remain fairly unchanged. A patient I saw told me that he noticed the pupil big when he looked in the mirror when he got up to go to the loo in the middle of the night but it was normal when he looked in the morning
- light reflex should be intact – the efferent part of this is mediated by the parasympathetics so should be unaffected in Horners
- get your sides right – a patient (or referring doc) might tell you they have a dilated left pupil when in reality it’s a constricted left pupil
What might I (ahem) you have mistaken this for in the past?
- the classic (in a conscious patient at least) differential for pupil asymmetry includes a posterior circulation aneurysm that’s putting pressure on the oculomotor nerve (III) in it’s rather taut course across the floor of the brain
- the parasympathetic fibres that control pupil contraction run in the peripheral part of the nerve so this is lost before the central fibres, controlling eye movements, are affected
- the more substantial levator palpebrae superioris is supplied by the oculomotor (III) nv on a somatic not an autonomic basis
- if you get your sides right (as mentioned above) you’ll be fine
Presentations you’d want to think about Horner’s in:
- stroke – while stroke is the end consequence of untreated carotid dissection, it’s important to know to make the diagnosis as you need contrast for the scan to pick it up
- headache – a headache and horner’s should make you at least think about a diagnosis of carotid dissecton
Final points
- CT angio probably the test you’ll get. There are lots of other ways to look for it too
- treatment is probably best with anti-coagulation. I’m not sure whether there’s a definite answer of warfarin vs heparin vs aspirin. The important point is to know that it’s different from aortic dissection where you definitely don’t want to anti-coagulate.


“These are carried as a plexus in the wall of the carotid artery.”
PEARL!!!
I didn’t know the plexus was actually in the wall of the carotid! COOL! [she says nerdily while pushing up thick glasses and adjusting her pocket protector].
Always love when blog surfing feels like studying…makes me feel a teeny bit less guilty (especially since my spotter is tomorrow). EEK!
went back and checked that one and I think it’s probably more accurate to say that the sympathetic fibres lie “on” rather than “in” the wall. they can be separated (with care)
this article might help http://www.ncbi.nlm.nih.gov/pubmed/1758594
and this diagram gives a good impression of the idea http://en.wikipedia.org/wiki/File:Gray844.png
apologies!
Hahah, I wasn’t trying to fact check you but thanks for the correction. Still, I didn’t realize they were that intimately connected–makes sense though.
Yeah I suppose one would require *great* care in separating the two! 🙂
This summer I had the opportunity to scrub in for some ENT surgeries and HOLY CRAP were they ever intense! I never had an appreciation for all the intricacies and tightly packed vital pieces of meat that are in the neck (a rather small space, really!) When I was told to hold the retractor ‘firmly but gently’ I could feel the sweat start to pour down the back of my legs, watching the carotid thump away. Crazy.
Pingback: More on Horner’s syndrome… | Emergency Medicine Ireland
this is very cool !!
i came across this blog when i was looking about horner’s syndrome.
and I found that your explanation was very brilliant, practical, and educating.
thanks a lot for sharing… =D