When I posted on airway management in the ED I included this video that I found via @movinmeat.
It’s a must watch. If you haven’t go watch it and come back.
[vimeo http://www.vimeo.com/970665 w=400&h=213]
There has been a recent and much welcomed surge in safety in medicine. Perhaps the most prominent of which has been the WHO checklist with authorship and widespread popular support from Atul Gawande. There is lots and lots of other stuff out there on this kind of thing.
Audit in all its beauty has driven us to examine us how often we cock up and why.
In the prior post myself, albinoblackbear and domnhall had a bit of a discussion about this type of thing.
Checklists are a great way to short-circuit one of the key human factors in error – personality. Perhaps personality is too PC. Arrogance and superiority are better words.
It’s great to see how the arrogance required to think that you don’t need to check the side for surgery is punctured like the balloon of hot air that it is by a patronising little check list that forces you to talk out loud.
I love it.
Checklists are here to stay it seems and I welcome it but reflecting on it makes me think that we’d also be wise to invest in relationships.
Now before you think I’m sitting here cuddled up with my teddy bear and my rose-tinted glasses let me try and clarify that a bit.
I tell a great number of my patients that medicine is not nearly as exact a science as they think it is.
I love EBM, I love the empiricsm, i love the science behind all that we do but in everyday practice (especially in the ED) the patients, systems and people we work with are not mere protocols to be followed.
My suggestion is that most of what we do it based on trust. As flawed and broken as that might be.
When a patient tells me something I have to trust them. Sometimes I don’t trust that they are telling me everything. I make a judgement call based on lots of things with virtually every patient.
A quick example. I describe patients as symptom minimisers and symptom maximisers. When it comes to chest pain most of my decision to admit or not is based on history. And patients don’t read the text books and I have to work out and make a judgement call on all kinds of variables, dynamics and personality aspects of the patient and the encounter I have with them. You do this everyday without thinking.
I trust the nurses. Put your hands up if you’ve had a nurse save your ass in the ED. OK you can put your hands down now.
While it’s not good to be wrong, it is a good and healthy thing to be able to be wrong in front of your peers.
I trust the nurses to do what I ask them and not just in the letter of the request but also in the manner in which it’s done.
I trust, indeed I depend on the nurses to put up a fight if I try to do something they think is wrong. I might still do it, and with good reason, but I trust them to at least make an objection.
I trust the docs I work with, from the juniors who ask me questions to the guys I refer the sick patients. I trust them that they won’t fuck it up.
Now of course I don’t always trust them, sometimes you need to have a stand up row with someone. Sometimes it’s important that we make the decision and not the nurse.
I have worked in the same hospital now for 11 years (4 as a cleaner at weekends during med-school and 7 as a doctor on and off).
I get a little bit weepy thinking about the place and the people.
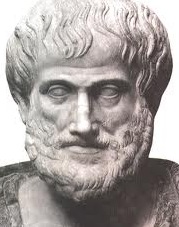
I have a friend who worte a masters thesis on friendship and Aristotle. Aristotle thought (when we’re talking Aristotle “thought” is not just some lazily put together opinion – like this blog for example…) that you couldn’t be virtuous or live well (eudaimonia) without friends.
My suggestion is that you can’t be (or at least it’s difficult to be) a good doc without good relationships.

Thanks for the shout out. And it is a particularly difficult to watch video, but inspiring in its way, isn’t it?
When I first watched it I was thinking he was going to tear the docs apart for getting it wrong but it’s so refreshing to hear him speak positively about lessons learned and their return to work. It make the whole idea so much more powerful coming from him.
Incidentally do you use checklists in your practice? I’ve only ever used them for central lines. They seem like hard things to implement in a chaotic emergent ED setting.