I mentioned these on Twitter a while back but I thought they deserved a little plug.
All hospitals have pretty good policies and procedures about what to do when a staff member gets a needlestick injury. A lot of these patients in the systems I’ve worked in come to the ED out of hours. It’s our responsibility to do a risk assessment and ensure the appropriate bloods and paperwork are done and in the rare occasion consider PEP.
Where I’m currently working in Dublin has a substantial population of IV drug users and we also receive patients from large prison across the road. It makes for an interesting population of patients. It also results in lots of blood born virus (BBV) exposures in the community setting.
These guidelines [free PDF here] give clear and specific guidance about what to do in each situation. They were put together by a whole bunch of people but there a few emergency physicians involved in the process too so it’s relevant to what we do.
There’s lots of useful info in it but here’s some highlights
- Hep B vaccine is highly effective at preventing infection if given ear;y (preferably within 48hrs) and they suggest a low threshold for giving it in any significant exposure. This is of course good news considering how tremendously infective Hep B is. There is a role for passive immunity from Hep B immunoglobulin but they confine it to “limited circumstances”
- There is no prophylaxis for Hep C (which is a shame considering how easily transmissible it is), however it’s still important to get them tested and followed up as early treatment is highly effective at clearing the virus.
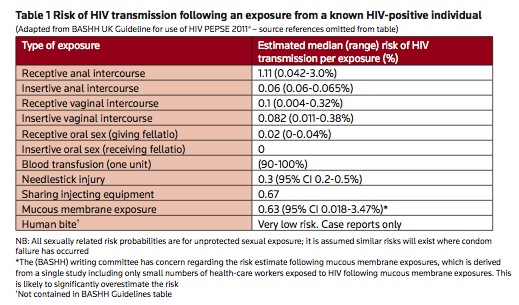
- HIV PEP should only be considered within 72 hours of the injury (hence the importance of the role of the ED when the ID guys are off for the weekend). To know when to give it requires a little sociology. Given the local population where I work, the majority of needlestick injuries are going to be sourced from IVDU and are fairly high risk so we use a reasonable amount of HIV PEP in these cases. Of note the number of people from occupational exposures (ie healthcare workers) who have seroconverted since the introduction of PEP is almost zero.
- Don’t forget tetanus
- Bites: “A recipient of a bite that breaches the skin but with no visible source blood does not require any follow-up from the point of view of HIV and HCV.” They do suggest Hep B
- Sexual exposure: In the case of sexual assault, Ireland has Sexual Assault Treatment Units (SATU) available but they may occasionally end up in your ED and the guidelines have a good algorithm for management.
There are lots of useful numbers to give you and your patient an idea of what the risk actually is.
And finally the tail end of the document has patient information leaflets, so that you can give the patient something home with them so they don’t have to remember all the information you just threw at them.
I’ve used the guidelines about once a week since I found them and I keep them as a PDF file on my phone so I can access them in work.
As a final plug there’s a one day conference launching the guidelines in Dublin on 19th April 2013 [Details below]
I’d be interested in how the guidelines match up to practice elsewhere in the world. If you’ve any thoughts leave them in the comments.
Conflicts of interest:
I have no financial or academic ties to these guidelines and I had no part in the development of them, however I do know some of the people who were. This post simply reflects the fact that I think they’re pretty useful for clinical practice.
UPDATE:
Graham Walker points out that there’s a nice risk estimator on the MD Calc site that’s worth checking out too.