This was fascinating to me, though it may be old news to some of you.
This paper1from WJEM is a narrative review of the available evidence used in forensic settings to link SDH and retinal bleeds with Non-Accidental Injury (NAI).
I have virtually no experience with this but like most I imagine, I thought that retinal bleeds and SDH in young children were near-pathognomonic of abuse.
The author challenges this and examines the original late 60s study that tested whiplash on monkeys and saw that it produced lots of SDH and neck injuries. His key point is that the forces needed to generate SDH would easily have broken the necks of the infants – something that does not seem to be a part of shaken baby syndrome (SBS). He makes a similar argument regarding retinal bleeds.
He argues for a different pathophysiologic mechanism of Intra-Dural Bleeding (from capillary as opposed to bridging veins) and retinal bleed from raised ICP and metabolic catastrophe.
All very interesting.
Then he describes this study2 that examined the incidence of SDH in new borns. In brief:
- they took asymptomatic healthy babies at >37/40 at birth
- each got US and MRI of their brains (none needed sedation apparently)
- images reviewed by radiologists
- those with bleeds got follow up scans (no intervention)
- evaluated at 2 years for developmental delay
they found:
- n = 101
- 80% vaginal deliveries, other c-section
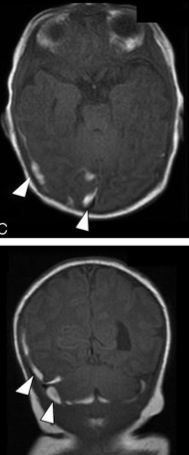
- 50% had SDH confirmed at follow up imaging (vast majority <3mm)
- most of the SDHs were in more than one location (most commonly para-falcine)
- when compared to MR, US missed a whole bunch (while no doubt true, it’s a little bit unfair as MR was the gold standard it seems)
- most were resolved by 4 weeks (not everyone got the follow up imaging as kids were fine and parents declined)
- everyone did great
In case you think these were tiny, invisible little bleeds, here’s some images for you.
As a sort of aside you can see why SDH happen if you check out this paper of someone giving birth in an MRI scanner and the images and MR Video (I’m not kidding) that goes with it. It helps you understand why you’re allowed a little bit of SDH following birth. It looks a little bit like this:
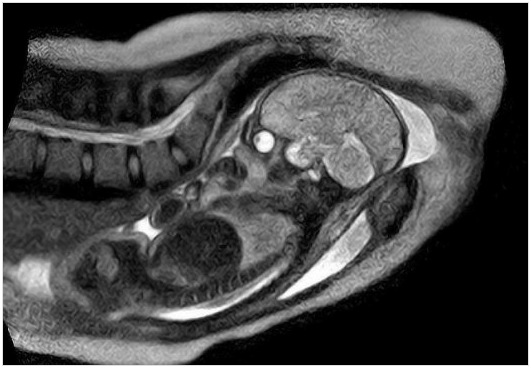
The paper3 with it has a great video you should check out if you have access to the journal. Here’s a YouTube edit of some stills:
The conclusion of the author of the first paper from this data is that SDH before 4 weeks of age might be birth related whereas after 4 weeks you need to think NAI.
Not sure if any of this changes practice but fascinating nonetheless.
Refs:
1. Gabaeff SC. Challenging the Pathophysiologic Connection between Subdural Hematoma, Retinal Hemorrhage and Shaken Baby Syndrome. West J Emerg Med. 2011 May;12(2):144–58. PMC3099599 (Free Full Text)
2. Rooks VJ, Eaton JP, Ruess L, Petermann GW, Keck-Wherley J, Pedersen RC. Prevalence and evolution of intracranial hemorrhage in asymptomatic term infants. AJNR Am J Neuroradiol. 2008 Jun.;29(6):1082–9. PMID 18388219 (Free Full Text)
3. Bamberg C, Rademacher G, Güttler F, Teichgräber U, Cremer M, Bührer C, et al. Human birth observed in real-time open magnetic resonance imaging. Am. J. Obstet. Gynecol. 2012 Jan. 13. PMID 22425409 (subscription required)

Pingback: R&R In The FASTLANE 020 • LITFL • Research and Reviews