Podcast: Play in new window | Download (Duration: 3:36 — 5.1MB)
Subscribe: Apple Podcasts | Spotify | RSS
Welcome back to the tasty morsels of critical care podcast.
As an EM trainee doing intensive care I will confess that I struggle to work up the enthusiasm to cover a nutrition guideline. With my deepest apologies to all the great ICU dieticians I have worked with, I just struggle to get excited over this stuff. Part of the reason for this is that our dieticians are so good I have cognitively outsourced the nutrition to them and have scraped together a knowledge basic enough to get me through the exam.
All that being said it’s worth being aware that there are some major pieces of guidance out there and you would do well to have a passing correspondence with them. I would highly recommend attending an excellent lecture given by your ICU dietician which is just possibly where this entire summary came from. This is certainly not intended to be a comprehensive review of ICU nutrition but a few pearls from the guideline.
Firstly nutritional assessment. This is the first step. ESPEN immediately embarks on a new cold war with their American colleagues by rejecting something like the NUTRIC score as definition of critical illness malnutrition stating nothing has been particularly well validated as yet.
They do stress the importance of assessing for malnutrition with some risk factors including
- BMI<20>40
- malnourished
- burns
- sepsis
- prolonged stay
- frailty
Depending on definition ~50% might be malnourished in ICU
They helpfully split critical illness into phases with regards to nutrition, which is probably the most useful thing I took away from the guideline.
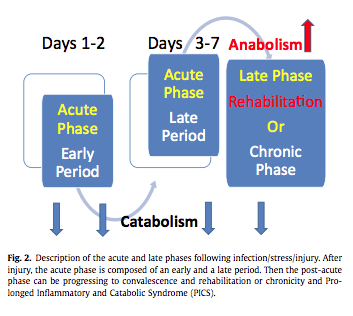
- The acute phase has an early period of instability and pressor use. Usually ~ 1-2 days when the body is very catabolic
- This is followed by a late period ~ day 3-7 where there is muscle wasting and stabilisation of metabolic abnormalities.
- Finally there is the late phase/chronic/rehab as the patient becomes more anabolic
According to this concept don’t rush to feed new admissions with increasing pressors or acute bleeding or life threatening hypoxia/acidosis.
As with all ICU nutrition EN is preferred over PN.
There are a few other points to take away from the guidance
Refeeding syndrome
- ~35% of ICU patients at risk of this
- drop in PO4 after starting feeds (drop of 0.65)
- prevention is typically IV or enteral thiamine and reducing rate of feeding.
Also important to remember other sources of kCal in the ICU
- propofol
- dextrose
- citrate
References:
Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, Hiesmayr M, Mayer K, Montejo JC, Pichard C, Preiser JC, van Zanten ARH, Oczkowski S, Szczeklik W, Bischoff SC. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019 Feb;38(1):48-79. doi: 10.1016/j.clnu.2018.08.037. Epub 2018 Sep 29. PMID: 30348463.