Podcast: Play in new window | Download (Duration: 5:15 — 7.5MB)
Subscribe: Apple Podcasts | Spotify | RSS
Welcome back to the tasty morsels of critical care podcast.
Like most spaces within the body, the contents within the cranium are under a certain degree of pressure. The skull being a rigid box can accommodate pressure much less than many other compartments in the body. The idea is that a modest increase in the volume of the box leads to a rapid increase in ICP. This is Monroe-Kellie 101.
It makes sense that we might want to measure the ICP as a target for intervention. What indications might we use for monitoring?
The BTF has guidelines on when to insert an ICP monitor that seem to be followed about as well as doctors adhere to hand hygiene. The list goes as follows.
- traumatic coma (3-8) with an abnormal scan
- traumatic coma with a normal scan
- if 2 or greater of: age>40; unilateral or bilateral motor posturing; BP<90
The normal ICP is usually 5-15 mmHg when we’re lying flat. We measure this fairly commonly in an indirect fashion when we check opening pressures at LP. The confusing thing is that we measure opening pressures in cm of H20 rather than mmHg. There is a conversion factor of 1.35 that I don’t find especially intuitive. However I have a tendency to remember it by the fact that any given number in mmHg will be bigger when in cm H20 which makes sense given that a cm is bigger than a mm.
ICP monitors typically placed in TBI patients will transduce a measurement in mmHg whereas we set EVDs in cm (even if they transduce in mmHg). All this is simply a reminder that the two are not the same.
While we have a variety of monitoring techniques we can use for ICP including clinical and ultrasound features, the main options we’ll see in a neuro ICU will be the EVD or the parenchymal ICP monitor.
A list of +ve and -ve features of each might go as follows (and deranged physiology has a much more detailed table)
EVD Pros
- gold standard
- can drain CSF (and therefore lower pressure)
- good measure of overall ICP
EVD Cons
- invasive – a big long metal needle is placed through your cerebral cortex aiming for the 3rd ventricle. There may well be important things in the path between the cortex and 3rd ventricle such as your wife’s birthday or that guitar riff from stairway to heaven that you spent so long learning.
- they can get infected (though there is frequently an element of neurosurgical denial that the EVD could be the source…)
- can measure or drain but not both at the same time
Parenchymal monitor Pros
- easier and more superficial to place
Parenchymal monitor Cons
- pricier
- measures the local parenchymal pressure that may not reflect overall ICP. For example a high reading might only reflect local oedema rather than brain ending herniation.
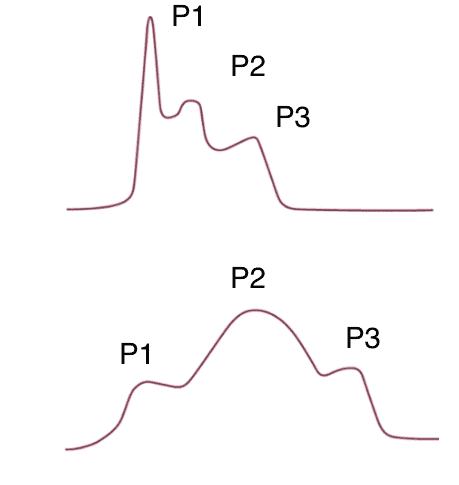
Like all monitoring devices they come with their own waveforms and are therefore very examinable. The ICP waveform consists of 3 separate spikes.
- P1 – pressure wave transferred from choroid plexus to ventricles
- P2 – “tidal wave” from brain compliance
- P3 – dicrotic notch of AV closure
While less than satisfactory in an audio format the image below shows a normal ICP waveform at the top with a staircase of decreasing spikes from P1 to P3. The lower image shows P2>P1 which reflects reduced compliance as the brain gets increasingly tight.
Finally there are waves known as Lundberg A waves that consist of spikes of ICP for 5-20mins where the pressure can go 50-100mmHg fairly randomly. This is a sign of failing cerebral auto regulation and are as you can imagine pretty concerning.
