[I suspect every emergency medicine blog eventually gets caught in the overwhelming gravitational pull of the VTE literature till it collapses into itself and sucks the whole of the internet into a wormhole. Apparently CERN is actually colliding the URLs of the EM blogosphere into one another to find the Higg’s boson. Or something like that…]
Smith, S B et al 2010. “Early Anticoagulation Is Associated With Reduced Mortality for Acute Pulmonary Embolism.” Chest 137 (6) (June 3): 1382–1390. doi:10.1378/chest.09-0959. PMID 20081101
Answer One – So you can get back to your life
Maybe? How the hell should I know?…
Answer Two – The slightly wordy hyperbolic rejection of the study’s conclusions
The above study shows compellingly that the administration of heparin the ED predicts pts with PE who are less sick
Answer Three – The, hopefully more nuanced and reasoned discussion…
Hat tip to Dr Weingart for alerting me to this paper
METHODS
- their question was whether timing of heparinisation was linked to mortality in PE pts
- chart review – dubious methods
OK, os that requires some qualification. You’ll recognise that’s Hoffman phrase. I’ll explain.
A chart review means that someone sits down with a chart they’re interested in and write down the bits that are relevant to the research question. No worries so far.
The problem is that when the doctor was writing the chart initially, they didn’t know someone would be sitting down with the chart later to try and answer a research question. As a result, lots of the time the information that the researcher is looking for isn’t there.
Even if it is there it’s hard to know what it means. The biggest problem comes here with subjective findings like symptoms, or the even more complex decision making process that goes on in a docs brain. These things aren’t always that clearly documented.
For that reason you need to be careful how you do it. There are recommended methods.
These guys didn’t do much of that. They didn’t tell us what they did about missing data (but it becomes clear there was a fair bit of it). They don’t get two people to look at the same chart and see if they agree.
Perhaps one of the most problematic issues is their calculation of a Well’s score. The gestalt/alternative diagnosis part is of course (as it should be) subjective and is going to be tremendously difficult to abstract from a chart unless they write out a Well’s score. Maybe they did this. They don’t tell us.
RESULTS
- 400 pts from a 3 yr period
- they say:
392 patients (98.0%) were accounted for by 30 days
I’m not sure what that means. Presumably that means they attended a follow up clinic. Or maybe it means they weren’t recorded as dead on the hospital system at 30 days. Again, they don’t tell us.
- 3% dead in hospital, 7.7% dead by 30 days
- pts who received heparin in the ED had a lower in-hospital mortality (1.4% vs 6.7%)
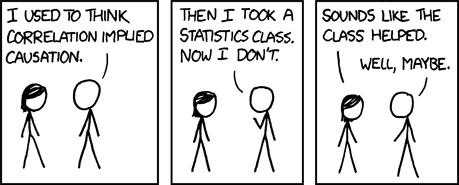
At this point a moment in honour of XKCD
People who get thrombolytics are more likely to die than those who don’t. Either thrombolytics are killing people OR people who get thrombolytics are having strokes and heart attacks and those who don’t are healthy.
Effectively that’s all that the statement “pts who received heparin in the ED had a lower in-hospital mortality (1.4% vs 6.7%)” can tell us. Either heparin given early is great OR people who got heparin earlier were less sick.
- the benefit for early heparin was maintained even after adjustment for co-morbidities
They say:
To account for comorbidities that would confound the relationship between the timing of anticoagulation and mortality, we calculated propensity scores and did subgroup analyses
Admission – I haven’t a clue how to calculate a propensity analysis. I am a half-(ass)-trained emergency doc who reads a lot. I’m still a bit dubious that you can account for significant differences between groups by statistics. This depends on knowing what the differences are. In the words of Donald Rumsfeld (Oh Lord, I’m actually quoting Donald Rumsfeld…)
There are known knowns, known unknowns, and unknown unknowns…
Propensity analysis can only account for the differences we know between the groups concerned. Correct me if I’m wrong on that – and it’ll not be the first time…
To give the authors credit they acknowledge this in the discussion:
Nevertheless, this was a retrospective study that did not have the advantage of randomization of patients to early vs late anticoagulation. Therefore, even with propensity score modeling, we can only demonstrate associations rather than prove cause and effect.
So why the difference in the two groups?
the folk who got treated later with heparin seemed to be more difficult to diagnose. It seems people admitted them thinking they were flares of COPD or MIs when actually they were PEs. They also seemed to be sicker overall (age being the main difference).
PE is a bugger of a disease to diagnose, and even to work out what a diagnosis means. Heparin may well help in PE, in fact I’m pretty sure it does for some people at the very least. And it may well help to give it early, at least in terms of hours or days as opposed to minutes (like tPA in MI). I’m just not sure this gives us the answer.
The most important learning point I would take home from this paper is that we miss PE on a frequent basis, especially, it seems in people with COPD or MI where we think we have the diagnosis sealed prematurely.
On the other hand we probably overdiagnose it in other people but that’s another story…


Pingback: mortality from pulmonary embolism