(featured image, JL Johnson on FLickr, CC license)
I’m entering a few months prep for the UK and Ireland exit exam in Emergency Medicine: the FRCEM. I’ll be adding lots of little notes on pearls I’ve learned along the way. A lot of my revision is based around the Handbook of EM as a curriculum guide and review of contemporary, mainly UK guidelines. I also focus on the areas that I’m a bit sketchy on. With that in mind I hope they’re useful.
You can find more things on the FRCEM on this site here.
Classes
- Amide
- Lignocaine
- Bupivacaine
- Priolcaine
- Esters
- Cocaine
- Benzocaine
- Tetracaine
[collapse]
How do they work?
- All work by
- “inhibiting sodium influx through sodium-specific ion channels in the neuronal cell membrane, in particular the so-called voltage-gated sodium channels.” (Wiki)
- Different pain fibres are affected in different ways with sympathetic fibres being most sensitive followed by pain fibres. Hence the sensory block without motor block that we often see.
[collapse]
Max Doses
- Bupivacaine 2mg/kg
- Lignocaine 3mg/kg
- Lignocaine with Adrenaline (1:200000) 7mg/kg
- Prilocaine 6mg/kg (of note remember the MetHb risk with this – I’ve seen it and been responsible for it!)
- NUH have a lovely table with patient weights and different concentrations all worked out.
- Also of note if you’ve given your 2mg/kg of bupivacaine you can’t just have a go with lignocaine
[collapse]
Discuss Local Anaesthetic Systemic Toxicity
(From the AAGBI 2010)
- Signs
- altered mental staus
- CV collapse, brady, conduction blocks, asystole and VF/VT
- apparently you can also get a rash (if you need a third body system for an exam question…)
- of note can be delayed
- Management
- Stop injecting the stuff dummy
- HELP!!!
- ABCs
- Stop the seizure with your agent of choice (benzo, prop, thio…)
- If cardiac arrest
- CPR
- Lipid Emulsion
- May take >1 hr for recovery so keep going!
- From the realms of the obvious
- propofol not a suitable substitute for intralipid despite being made from it
- don’t give lignocaine for arrhythmias
- (sigh… eye roll… repeat)
- If no cardiac arrest
- supportive yadda yadda
- consider lipid emulsion
How to give the intralipid
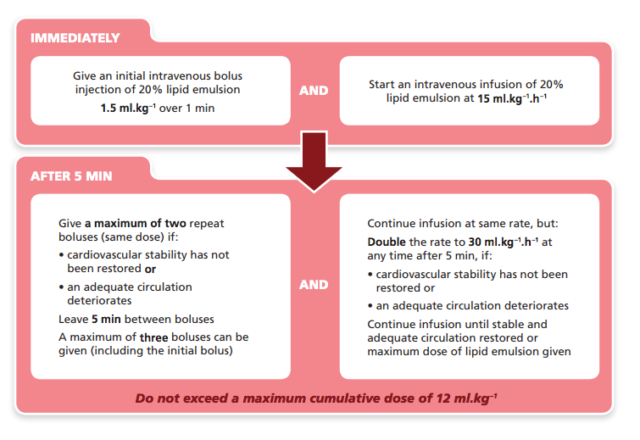
- Bolus
- 20% intralipid 1.5ml/kg over 1 min (eg about 100mls in a 70kg patient)
- Can be repeated twice (once every 5 mins)
- Infusion
- as soon as the 1st bolus given
- infusion of 15ml/kg/hr (1000ml/hr of 20% solution in a 70kg patient)
- if repeating the bolus then double the infusion rate
- 12ml/kg of the 20% is the maximum dose
[collapse]
