Podcast: Play in new window | Download (Duration: 5:13 — 7.5MB)
Subscribe: Apple Podcasts | Spotify | RSS
Welcome back to the tasty morsels of critical care podcast.
Today we’re not so much looking at a chapter of Oh’s manual but at the physiologic concept of respiratory compliance. I approach this with a degree of trepidation as the probability of screwing this up is infinitely higher than simply translating Oh’s manual into podcast form.
Compliance is relatively simply defined as change in volume per change in pressure. Put another way, for every 1 cmH20 pressure i apply with the ventilator I get 100mls of volume. The compliance in this scenario would be 100, ie 100 divided by 1 = 100. 100ml/cmH20 also happens to be normal compliance of the human lung. You’ll sometimes see compliance written as delta volume divided by delta pressure.
There are a few different types of compliance described for the respiratory system.
- static compliance = compliance in the absence of flow. This consists of the compliance of the lung tissue and the chest wall and is the number we look at generally
- dynamic compliance = compliance in the presence of flow. This consists of chest wall and lung tissue compliance AND airway resistance (and will always be lower than static compliance)
- specific compliance = compliance normalised for lung volume (kind of like an indexed value so adults and kids can be compared)
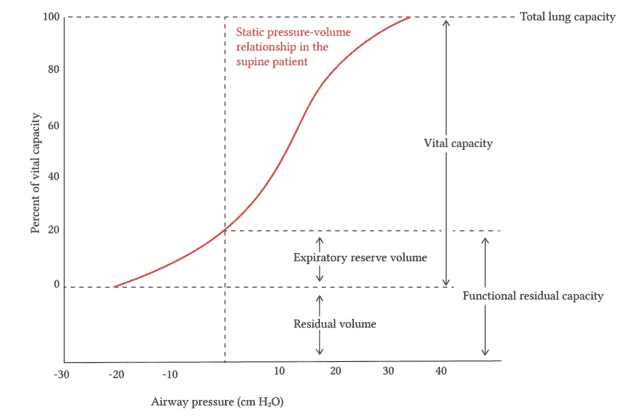
Compliance will vary depending on distension of the lung with ideal compliance usually just above the FRC. When overdistended and about to pop, you can imagine that increases in pressure will only produce small changes in volume. The same is true when the lung is at very low, atelectactic volumes where the lung tissue is squished solid and large changes in pressure are needed to produce a change in volume. This is nicely represented in the graph from deranged physiology in the show notes that shows a nice sigmoid curve of lung volume plotted against airway pressure. The steep part of the curve represents the ideal compliance as you get the most “bang for your buck” in that small increases in pressure will result in substantial increases in volume.
We are very interested in lung compliance in the intensive care unit. We talk a lot about stiff lungs and spend a lot of our time and energies trying to optimise ventilation of those with poor compliance. So how do we measure or assess compliance?
This becomes a sort of reflex over time where you simply walk in the room and look at the vent and the driving pressure and the tidal volume produced and a synapse somewhere ignites and tells you that 25cmH20 pressure to produce 250 mls of tidal volume is not good. If you do the basic calculation of delta volume divided by delta pressure, of 250/25 you get 10 which is indeed a very low compliance and of great concern. This is most of what you need to know for day to day practice.
However for examinations of brownie points you might wish to know more and understand many of the circumstances where that kind of heuristic might be wrong.
The gold standard is apparently something called the super syringe method which involves inflating the lung in 100ml increments with a 2-3 sec pause at each inflation. This measures static compliance and i mention it mainly cause it has a cool name.
In real life we measure compliance by fiddling with the inspiratory and expiratory hold buttons and looking at what the ventilator spits out. This is technically the compliance of the respiratory system rather than true static compliance but I remain somewhat in the dark as to the subtleties of the difference.
What you do with the number is a whole different question. Stiff lungs do worse. That’s hardly a surprise. Given that compliance is typically best just above the FRC we can titrate PEEP to idealised compliance. This is best explained on a critical care now post by Matt Siuba, linked in the show notes. The basics of this involve a passive patient in a volume control mode and the PEEP is dialled up and down with a fixed volume to see at which PEEP you get the best driving pressure (ie the lowest amount of pressure to produce the set volume). This should place you on the steep part of that curve and just above the FRC.
There are actual a number of methods trying to attain the same thing and I don’t mean to imply that this is proven best but I have put a few links in the show notes for those looking more and will hopefully do a whole post on setting PEEP and recruitment at some point.
Reading
Sahetya, S. K., Hager, D. N., Stephens, R. S., Needham, D. M. & Brower, R. G. PEEP Titration to Minimize Driving Pressure in Subjects With ARDS: A Prospective Physiological Study. Respiratory care 65, 583–589 (2020).
