I’m entering a few months prep for the UK and Ireland exit exam in Emergency Medicine: the FRCEM. I’ll be adding lots of little notes on pearls I’ve learned along the way. A lot of my revision is based around the Handbook of EM as a curriculum guide and review of contemporary, mainly UK guidelines. I also focus on the areas that I’m a bit sketchy on. With that in mind I hope they’re useful.
You can find more things on the FRCEM on this site here.
Interestingly I’d written about this 4 years ago reviewing a series of AFJEM articles. It’s all still very relevant and worth a look but this is a little update for the exam specifically. This is of course not comprehensive.
From the OHEM and the 2011 BAHIV guidelines
- Fungal
- Only found in the immunocompromised
- usually in CD4<200
- Insidious onset over weeks with SOB on exertion
- LDH usually >500
- If you’re lucky CXR looks like this:
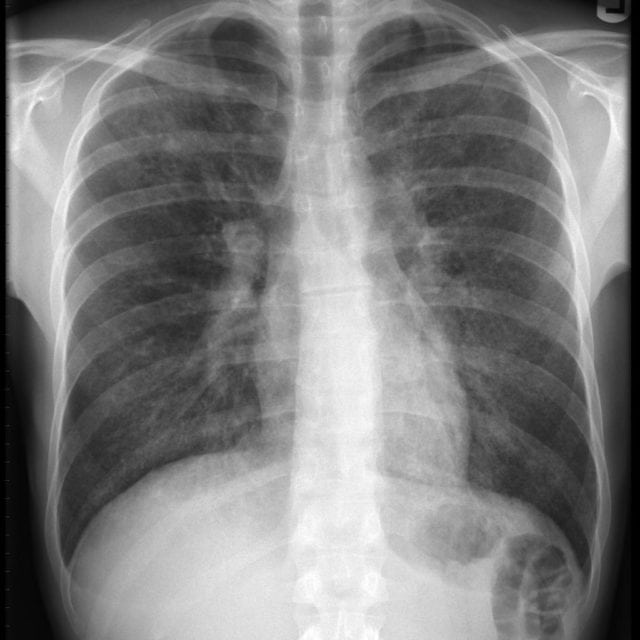
- Or you might find a pneumo but it can be fairly normal (quoted in up to 40%)
- Exertional desaturation is useful (what do you mean you don’t walk your patients in the ED?!?)
- Treatment
- the key threshold is PaO2 <70mmhg (or 9.2kPa)
- If below threshold then IV co trimoxazole and steroids (40mg BD prednisolone)
- If above the threshold then oral co trimoxazole
- Headache, fever, usually without neck stiffness
- Remember headache with HIV is a reason to do a CT before LP
- Fungal
- ICP is often high so expect vomiting
- Treatment
- amphotericin B
- LP can be therapeutic. If pressure >25cmH20 then keep draining till below 20cmH2O
- A protozoa
- cat poo the famous way to get it
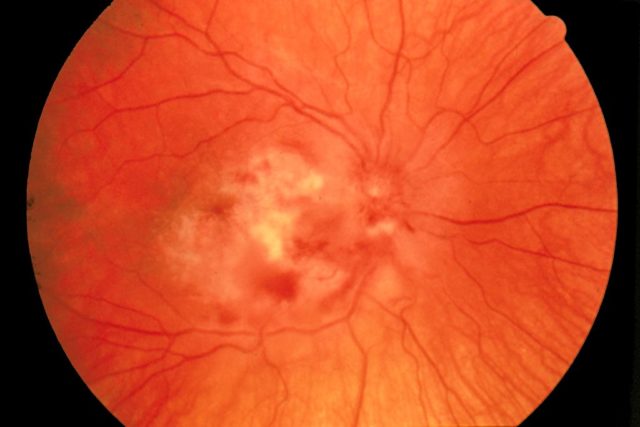
- Eye disease

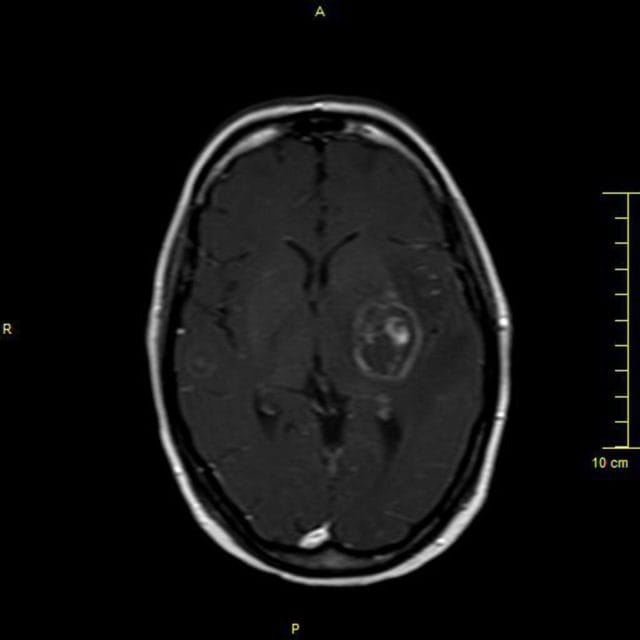
- Brain disease
- Might look like this:
- usual eye symptoms
- blurry
- flashers
- floaters
- can cause detachment
- might look like this