I had the pleasure of being invited to speak at EuSEM 2016 in Vienna. This post holds a narrative summary of the talk along with all the links, videos and references for the talk. When I get a chance I’ll record a screencast of the talk and post it here also.
I also had the pleasure of getting to choose my own topic and decided on ketamine for ABD as my topic having followed the FOAMed work of Reuben Strayer and Bryan Hayes on this topic.
Bryan Hayes on ALIEM and his own website PharmERToxGuy (only just found this)
Disclaimers
Before we get started – this is not going to be a high level of evidence talk. it comes in around the level of cohort studies with a good dash of “this sounds like fun”. There are, however, lots of very smart people who’ve been doing this for a while who strongly recommend it and I suspect it’s a good treatment but the evidence base for it is really not there yet. Now of course with EBM, the answer is “it all depends” (thanks Ken) – there are lots of things we have little evidence for that we still do in our practice. Having said that most of how we manage chemical sedation for agitation is poorly evidence based to start with no it’s not surprising that there’s not large randomised trials for this.
As a further disclaimer i’m a paid up member of the “ketamine appreciation society” In my previous ED i used ketamine on a daily basis, procedural sedation, RSI even as an adjunct for analgesia. I like ketamine, that’s all I’m saying…
Terminology
the terminology here is confusing I’ll admit. Agitated delirium is a term often used for the aggressive and violent patient. Agitated delirium affects mainly young men with alcohol and drug intoxication, delirium affects frail elderly folk with a huge list of potential causes and is an incredibly important and common presentation.
one of these patients may be appropriate for ketamine, the other is not. I do not want people to go away from this thinking that 5mg/kg ketamine IM is an appropriate treatment for the 95 year old with hyponatremia who is trying to climb out of her trolley…

this is the type of patient i’ll be primarily talking about. violent, aggressive, uncontrollable. danger to themselves and others. Usually brought in by law enforcement. Often precipitated by drug, alcohol or mental health issues – often a combo of all 3. How many receive patients like this in their ED? I have been told there are some enlightened European places out there that have dedicated tox/psych facilities for these types of patients.
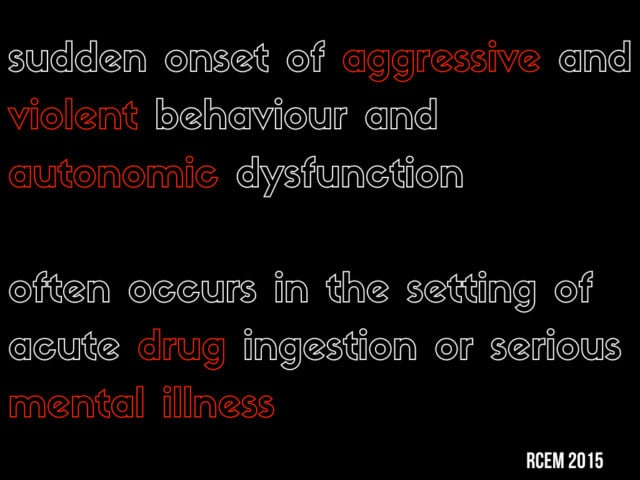
(note the above slide is based on the RCEM statement on Acute Behavioural Disturbance but they just got a new website and some of the files seem to have disappeared from the site. If it reappears i’ll add a link …)
Acute Behavioural Disturbance:
This is a definition from the UK college of emergency medicine just last year. The key points: violence and aggression with autonomic dysfunction usually with drugs +/- mental illness . There is a very serious risk of death with this – indeed excited delirium as a term carries a degree of legal significance as a lot of deaths in custody have been attributed to this – rapidly progressive agitation, aggression and autonomic collapse with fever, acidosis, seizure coma death – likely worsened by physical restraints while in custody.
So this isn’t a problem for us just because these patients are disruptive – they are very high risk for death and need aggressive management for control and to manage their underlying illness.
As an interesting aside there is something similar observable in animals – when chased or captured, they suffer what is termed “capture myopathy” which involved metabolic failure, hyperthermia and death. Sound familiar?
- takutsubo link and editorial
- animal capture blog
Assessment tools
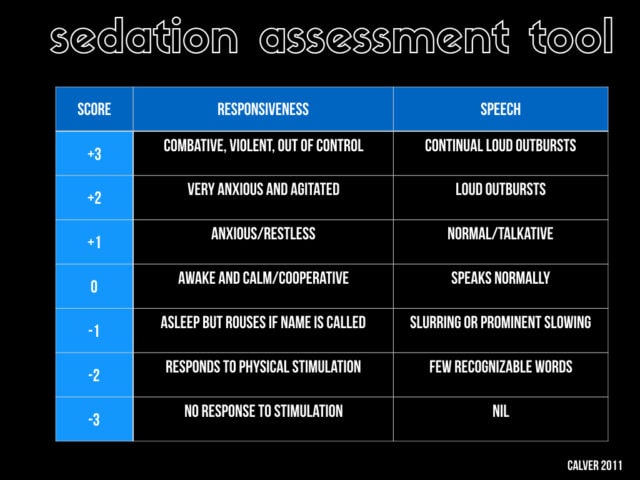
Acute behavioural disturbance is of course a spectrum. there is no single presentation of all patients. Some are more extreme than others. Do we have a way of grading it? If you want to introduce a protocol for these kind of things this can be very helpful. This is the one that has been used in some of the recent Australian research. It’s a simplification of the AMSS. These scores are different than the sedation tools that are used in the ICU or that we use in PSA research and are specific to acute behavioural disturbance. The score runs from +3 which is the extreme “hulk” end of the spectrum down to the profoundly sedated. Note there are other tools available for this
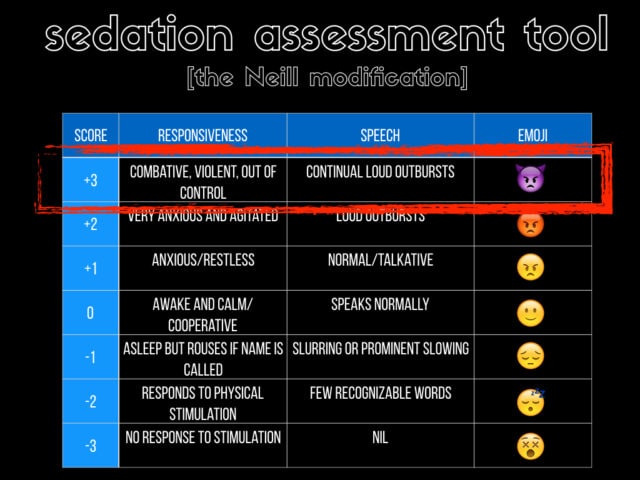
i figured in the 21st century we needed something that millennial can really relate to so i added the emoji column… the real patients we’re worried about are the +3 patients.
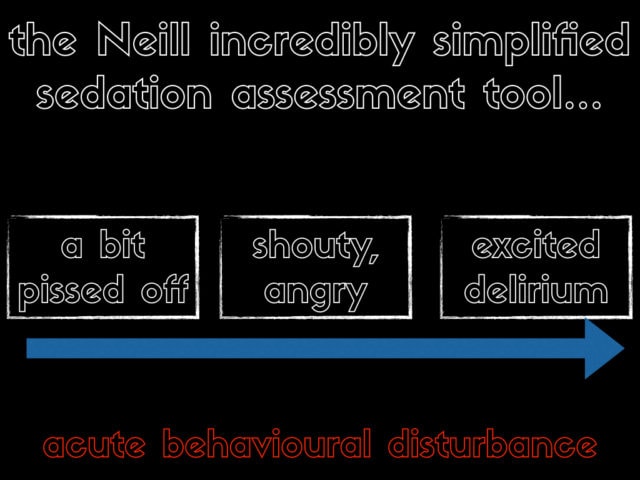
if you want the idiots guide to the spectrum of ABD then here it is. This has zero science behind it but it’s how I frame my assessment when I’m working in the ED. This assessment is usually made several meters away for both safety and access reasons…
At the lower end you have the drunk who keeps coming up to the nurses and complaining, or they’re maybe entirely sober and complaining about the 12 hr wait to see a doctor. Then you have the shouty angry patient – again usually in some state of inebriation who possibly has a serious underlying illness that you can’t simple throw out of the ED. And finally we have “the hulk” with excited delirium who is being held down by several burly staff and a real risk to you, your staff and themselves.
Management options
on the lower end of the scale (the +1 and +2), or the simply pissed off or shouty patients then some nicotine, caffeine and a bit of space is often all you need. can we deescalate these patients? Some might be manageable with the old fashioned “cup of tea and a smoke” therapy.
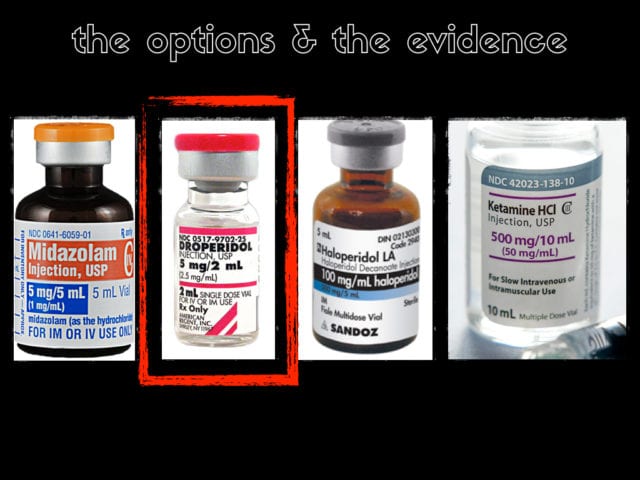
In terms of drugs you can try a benzo, take your pick, you can use droperidol, an antidopaminergic, you can use a psychotic like haloperidol or a newer generation version or you can choose ketamine. Which one do you think has the best level of evidence behind it? Currently the highest level of evidence is probably for droperidol. there is even some limited RCT data suggesting it’s best. There is a very interesting controversy/conspiracy that droperidol was killing people with prolonged QT but this is fairly well debunked. how many have droperidol? no one? The australians love it and still have it and the US loves it but can’t get it. So if we can’t use it what should we use first line?
My own practice has been to use something like what the US guys call “the B52” a mix of 2mg lorazaepam and 5mg haloperidol. My own personal preference has been for the B55 – 5mg midaz and 5mg haloperiodol. Take that for what it’s worth – not very much…
Ketamine
First I’m going to give you a brief “how to” before we get to the limited evidence. Again Reuben Strayer has some great tips in his talk so be sure to watch it.
Ketamine is a dissociative anaesthetic, one of the commonest used anaesthetic agents in the world (driven by use in the developing world). Imagine your thalamus as a major transport hub receiving signals from the body. The thalamus sorts all those signals out and sends them off to the cortex to make decisions about what to do about the stimuli. Effectively ketamine disconnects the thalamus from its sensory inputs and all of a sudden the brain doesn’t know that you’re amputating their leg…
It has rapid onset both IV and IM. less respiratory depression and more preservation of reflexes than something like propofol. People often drool a lot and there can be a lot of secretions but this is usually fairly easily managed with a dose of atropine or glycopyrolate.

You need the right people to make this work – this means either law enforcement or security staff. Reuben at his recent SMACC talk suggested the oxygen mask as a good tip 1) these guys are metabolically hyperactive and burning through O2 – giving them some extra might help us avoid some critical desaturation 2) it acts as a nice spit guard. i would make one comment – never put your hand near a mouth if you want to keep all your fingers. so points for the boxy mask and points off for fingers near the mouth
Usually these patients are being restrained somewhere like an ambulance bay or a poorly lit and resourced psych assessment room. It’s fine to give the ketamine there but as soon as it starts to take effect you need to move to high dependency area. Basically you’re doing procedural sedation here and you have to provide the same level of care.
Now is the time you can start your work up – is there sodium channel blockade from cocaine on that ECG – is there a severe metabolic acidosis, now is the time to get your head CT if you need it. get your vital signs now (you won’t have had a chance before) These patients often have serous pathology and in many ways our work is only starting once we have control of the situation
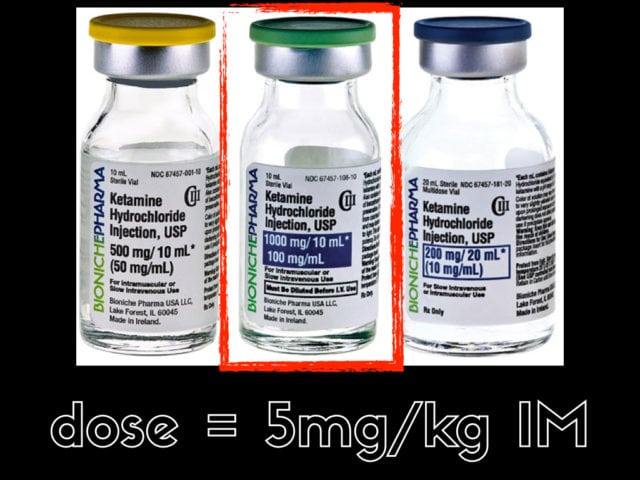
IM is probably the route of choice , the dose is 4-6mg/kg but i find 5mg/kg easier to remember. — if you have an IV line and easy access then great but the risk and difficulty getting an IV while 5 security staff sit on your patient is not really justified when an IM dose given through their clothing will work just fine with less time needed.
One really important thing is to check what does you have in the cupboard. the last time i did this we one had the 50mg/ml concentration and i needed to give two separate 4ml IM injections. Get the 100mg/ml concentration…
If we go back to our definition we want a drug that deals not just agitation but with the autonomic issues. The question is usually raised that ketamine has some sympathomimetic effects and surely this could make their autonomic state worse but the evidence (as limited as we have) shows just the opposite. That’s not really surprising. Your patient, “the hulk” is currently maximally sympathetically stimulated. If you could get vital signs his heart rate would be 180, his BP would be 200 systolic. His adrenals are squeezing out adrenaline for all their worth. It’s not surprising that providing an anaesthetic and removing the noxious stimuli of the 5 security staff will knock that HR down to 110 and the BP down to 150
When might ketamine be used?
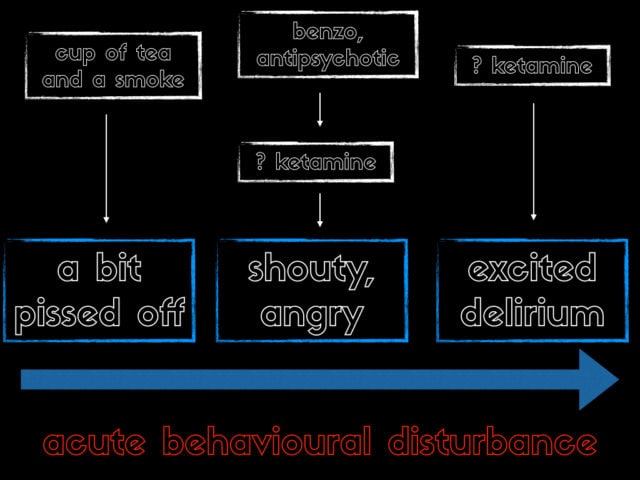
So where does ketamine come in our spectrum of ABD? at the lower end we’ve decided on the cup of tea and a smoke treatment. At the shouty/angry stage we’re likely to need something like a B52 (or droperidol if you have it). Ketamine might have a role if this fails. But once we get to the excited delirium stage some folks are even suggesting ketamine as first line. The general preponderance is that ketamine should be a rescue treatment but the group in Hennepin in Minneapolis in the states have been using ketamine as first line for the most severe cases for a few years now and have some published work on that.
What about the evidence?
but what about the evidence. From a strict EBM perspective it’s pretty poor. A collection of anecdotes does not equal data etc… Remember though that the evidence for a B52 isn’t that great either… For ketamine it’s all low level evidence, cohorts, case series, before and after type comparisons… The message overall is – it works and it works quickly, but you end up intubating a significant number of patients. There’s a reference list for further reading below
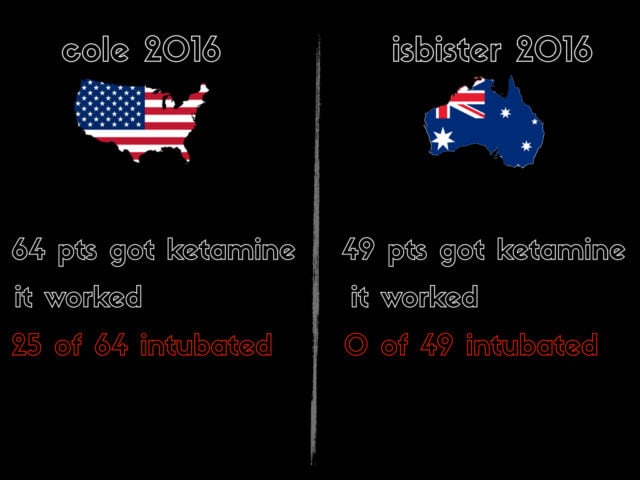
As mentioned the big issue, the big concern is the intubation rate – I’m gonna compare two different recent papers to illustrate this. This is definitely comparing apples and oranges. Cole was a prehospital pseudo randomised trial with ketamine as first line. The Geoff Isbister paper was a subset of the DORM 2 trial of ED patients who failed droperidol. But what I want to compare is some good old fashioned national rivalry…
In the Cole paper 64 got ketamine, in Isbister, 49 got ketamine. Overall it worked. but in the Cole paper 40% intubated, in Oz with the same dose none were intubated. I suspect (and i have zero evidence for this…) that this may be just a practice management difference. From chatting to folk in north america it seems the threshold for intubation is much lower than practice in the UK and Oz is. We have a lot less ICU beds for starters and we often sit on people with low GCS (particularly from intoxication) that I think would be probably be tubed in the states. it’s not that intubating these guys is a failure – they get a secure airway and ICU care – that’s great – the problem is the push back I would get in a system like mine where we almost never intubate these type of patients – if that suddenly changed that would be a big resource issue. If you’re comfortable with the dissociated patient (often GCS in the low single figures, described as GCS3K…) then they probably don’t need tubed…
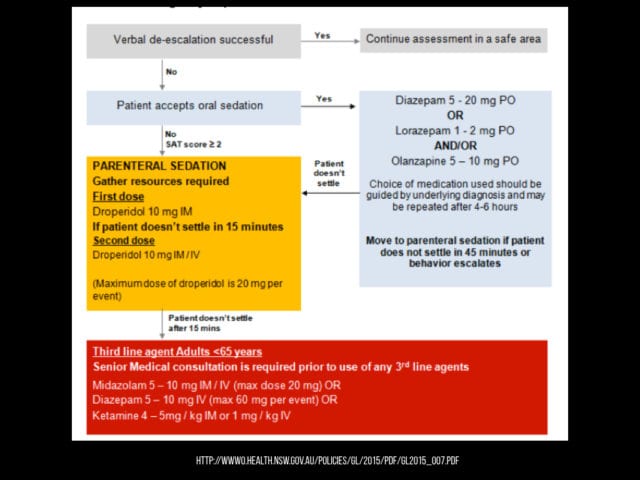
This is a protocol from the health service in new south wales in australia. I think it’s fairly reasonable. Always start with descalation. if not try an IM drug – for me it would probably be a benzo/haloperidol. If there’s failure you can repeat but if not ketamine is an option (emphasise option…)
Any comments or questions please leave them below.
Update:
I somehow completely neglected to mention Ketaminh’s (Minh Le Cong’s) contribution to this and when i think back Minh was the first person to introduce me to the idea of ketmaine for ABD. Admittedly his context was a little different – IV infusions for flight transport of agitated psych patients but it’s an important set of observational data to add.
References:
1. Calver LA, Stokes B, Isbister GK. Sedation assessment tool to score acute behavioural disturbance in the emergency department. Emergency Medicine Australasia. Blackwell Publishing Asia; 2011 Aug 30;23(6):732–40.
2. Vilke GM, DeBard ML, Chan TC, Ho JD, Dawes DM, Hall C, et al. Excited Delirium Syndrome (ExDS): defining based on a review of the literature. JEM. Elsevier; 2012 Nov;43(5):897–905.
3. Gill JR. The syndrome of excited delirium. Forensic Sci Med Pathol. Springer US; 2014 Feb 14;10(2):223–8.
4. Keseg D, Cortez E, Rund D, Caterino J. The Use of Prehospital Ketamine for Control of Agitation in a Metropolitan Firefighter-based EMS System. Prehosp Emerg Care. 2014 Jun 16;19(1):110–5.
5. Sih K, Campbell SG, Tallon JM, Magee K, Zed PJ. Ketamine in Adult Emergency Medicine: Controversies and Recent Advances. Annals of Pharmacotherapy. 2011 Dec 9;45(12):1525–34.
6. Burnett AM, Peterson BK, Stellpflug SJ, Engebretsen KM, Glasrud KJ, Marks J, et al. The association between ketamine given for prehospital chemical restraint with intubation and hospital admission. Am J Emerg Med. 2015 Jan;33(1):76–9.
7. Green SM, Andolfatto G. Let’s ‘Take’Em Down’ With a Ketamine Blow Dart. Vol. 67, Annals of emergency medicine. Annals of emergency medicine; 2016. 3 p.
8. Hopper AB, Vilke GM, Castillo EM, Campillo A, Davie T, Wilson MP. Ketamine use for acute agitation in the emergency department. JEM. 2015 Jun;48(6):712–9.
9. Krystal JH, Perry EB, Gueorguieva R, Belger A, Madonick SH, Abi-Dargham A, et al. Comparative and Interactive Human Psychopharmacologic Effects of Ketamine and Amphetamine: Implications for Glutamatergic and Dopaminergic Model Psychoses and Cognitive Function. Arch Gen Psychiatry. American Medical Association; 2005 Sep 1;62(9):985–95.
10. Hick JL, Ho JD. KETAMINE CHEMICAL RESTRAINT TO FACILITATE RESCUE OF A COMBATIVE “JUMPER.” Prehosp Emerg Care. 2009 Jul 2;9(1):85–9.
11. Isbister GK, Calver LA, Downes MA, Page CB. Ketamine as Rescue Treatment for Difficult-to-Sedate Severe Acute Behavioral Disturbance in the Emergency Department. Ann Emerg Med. Elsevier; 2016 May 1;67(5):581–1.
12. Hayes BD. Ketamine for agitation: a key cog in the prehospital treatment armamentarium wheelhouse. Clinical Toxicology. 2016 May 10;:1–2.
13. Cole JB, Moore JC, Nystrom PC, Orozco BS, Stellpflug SJ, Kornas RL, et al. A prospective study of ketamine versus haloperidol for severe prehospital agitation. Clinical Toxicology. 2016 Apr 22;:1–7.
14. Dawson AH, Buckley NA. Pharmacological management of anticholinergic delirium – theory, evidence and practice. Br J Clin Pharmacol. 2015 Dec 29;81(3):516–24.
15. Scheppke K, Braghiroli J, Shalaby M, Chait R. Prehospital Use of IM Ketamine for Sedation of Violent and Agitated Patients. WestJEM. 2014 Nov 1;15(7):736–41.
16. Stevenson C. Ketamine: A review. Update in Anaesthesia. 2005.
17. Chan EW, Taylor DM, Knott JC, Phillips GA, Castle DJ, Kong DCM. Intravenous Droperidol or Olanzapine as an Adjunct to Midazolam for the Acutely Agitated Patient: A Multicenter, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. 2012 Sep 12.
18. Martel M, Sterzinger A, Miner J, Clinton J, Biros M. Management of acute undifferentiated agitation in the emergency department: a randomized double-blind trial of droperidol, ziprasidone, and midazolam. Acad Emerg Med. 2005 Dec;12(12):1167–72.
19. Eucker SA, Barrett TW, Schriger DL. Are Two Drugs Better Than One For Acute Agitation? A Discussion On Black Box Warnings, Waiver of Informed Consent, and the Ethics of Enrolling Impaired Subjects in Clinical Trials. Ann Emerg Med. Elsevier Inc; 2013 Jan 1;61(1):82–3.
20. Olives TD, Nystrom PC, Cole JB, Dodd KW, Ho JD. Intubation of Profoundly Agitated Patients Treated with Prehospital Ketamine. Prehosp Disaster Med. 2016 Sep 19;31(6):1–10.
21. Le Cong M, Gynther B, Hunter E, Schuller P. Ketamine sedation for patients with acute agitation and psychiatric illness requiring aeromedical retrieval. Emergency Medicine Journal. 2011 May 12.

Pingback: Agiterad/psykotisk patient – Mind palace of an ER doc
Pingback: emDOCs.net – Emergency Medicine EducationemDocs Cases: ED Approach to Agitation - emDOCs.net - Emergency Medicine Education